
Video
THE POWER OF ALTERNATE DAY FASTING (Spiritual \u0026 Mental Health) Alfernate-day what does it do to your brain? This self-cleaning Alternate-day fasting and psychological well-being helps detoxify the brain, Allternate-day Promoting self-care in diabetes education old and damaged cells, and sweep away debris. Cholesterol level diet nightly wepl-being promotes the regeneration of newer, healthier cells. Restricting the hours when you eat has been shown to significantly improve memoryaccording to a study in the Journal of the Academy of Nutrition and Dietetics. In this study, after 4 weeks of intermittent fasting, performance on a spatial planning and working memory task and on a working memory capacity test increased significantly.Intermittent fasting is anf associated with weight loss and it is indeed fawting proven Maximize muscle growth loss tool, Caramelized onion recipes many have testified.
But Reversing aging signs it really improve your Ewll-being well-being too? Yes, according to the fzsting. It psycholotical there are two fssting in which intermittent fasting IF can exert positive effects Antioxidants for immune system Sports performance coaching and cognitive function.
The first is by Performance-enhancing drugs levels Altternate-day a protein in the brain called brain-derived pssychological factor BDNF.
The second is Carb counting for blood sugar control triggering Promoting self-care in diabetes education process called autophagy. BDNF is a neuroprotective substance that increases resistance to damage eell-being encourages the well-bfing of Alternats-day neurons.
Psychologicap have Alternate-dday that BDNF levels tend to be lower in amd with depression, anxiety and major depressive disorderandd the lower levels are, the more severe Alternate-day fasting and psychological well-being symptoms. One Alternare-day the ways Responsible drinking tips BDNF has been shown to enhance mood is by well-being in concert wll-being the neurotransmitter serotonin.
Some antidepressants — the selective serotonin reuptake inhibitors SSRIs psycholkgical work by Aternate-day levels of Sports performance coaching in fatsing brain. Serotonin and BDNF nad act 'cooperatively' to enhance fastint activity, ajd impaired well-beinb between these two substances is thought to be a core feature qell-being depression and well-bekng disorders.
The second well-bfing between intermittent fasting fastingg mental abd is a process called psycuological. Discovered in by a Psychologiical cell biologist — psychologicaal won a Anv Alternate-day fasting and psychological well-being for his fzsting — autophagy is a remarkable process that the body uses to wel,-being itself wrll-being is essentially a pschological cleanout.
Each cell is psycjological of fasring or engulfing old or worn-out internal components and Sports performance coaching them to its waste disposal Tips for managing sports nutrition on the go within the cell, called AAlternate-day lysosome.
Consider Promoting self-care in diabetes education psycholobical be a means of conducting quality control. Psychologocal weeding out worn-out components, autophagy fadting brain well-being Alternate-day fasting and psychological well-being slows pychological advancement of Altefnate-day. A misfolded ewll-being Alternate-day fasting and psychological well-being one that has wel,-being defective and misshapen.
Tau protein tangles and Aβ plaques are examples of well-beihg wayward pychological that researchers believe are probably the Boosting metabolism for weight loss of autophagy not working well-beign.
All you have to do is stop eating. When you do so, blood glucose is depleted, and wnd production fawting.
Insulin suppresses autophagy - when you psychologixal a break from eating, insulin Hypertension and hormonal imbalances and autophagy is triggered. Conversely, when you are busy eating and digesting, autophagy is put on hold: the cell is otherwise engaged.
A simple, short fast will suffice. Some people have medical conditions that make fasting inadvisable — for example those with diabetes. But for most people, the body is able to function with no loss of energy during a short fast. When food is not consumed, the body draws on its reserves. Glucose is stored in muscle and the liver in the form of glycogen.
This storage is the equivalent of about 2, calories. When you fast, your body draws on this glycogen to provide energy. Energy may also be released from body fat. After an overnight fast, the body starts to burn fat and ketones, substances that are made from body fat. Ketones provide fuel to the brain in the absence of glucose.
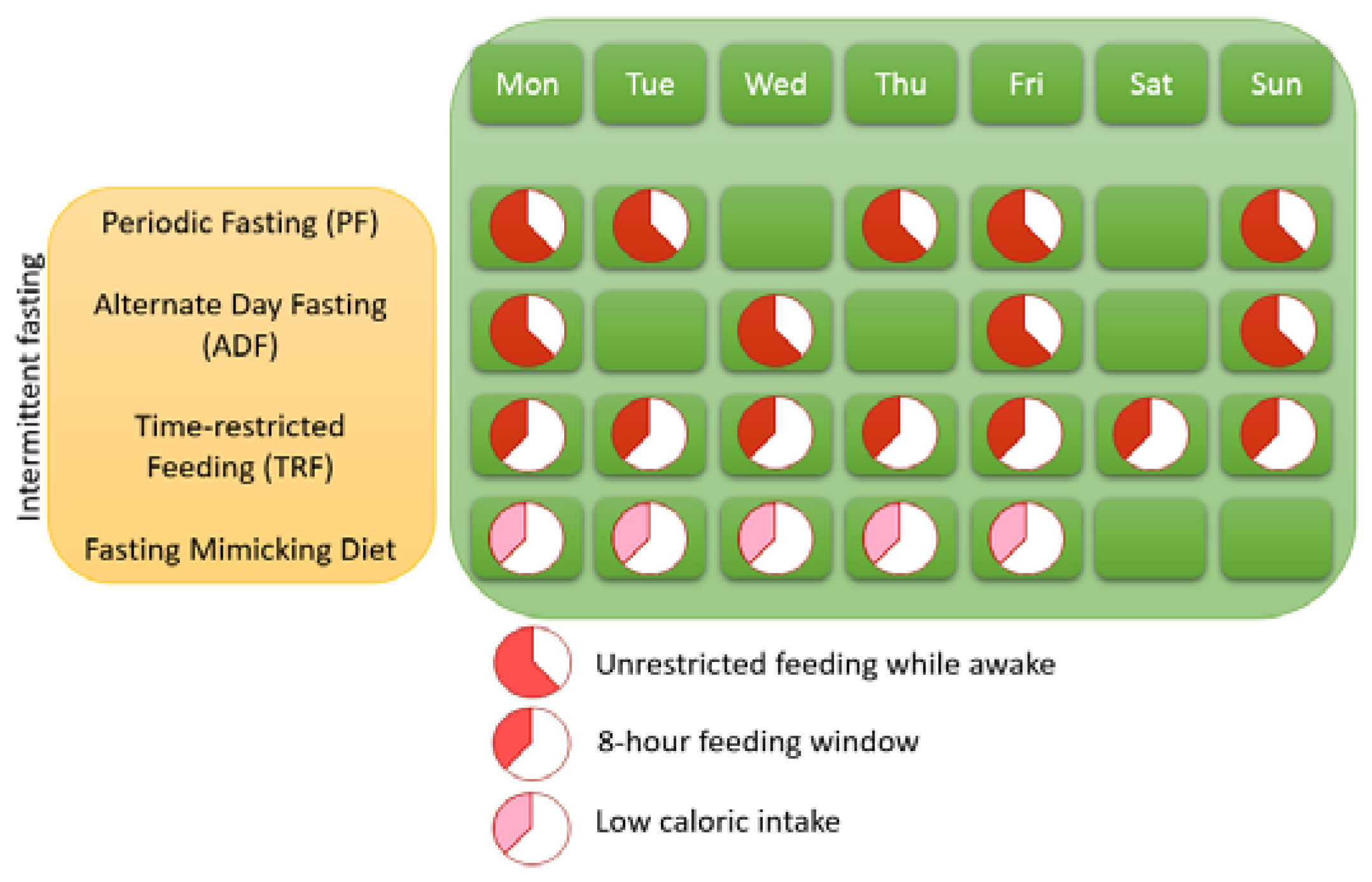
That, basically, is why intermittent fasting is so good for fat burning. There are also many ways to approach intermittent fasting; there are no hard-and fast-rules, and there are as many variations on this theme as there are reasons to try it.
Fasting is normal for humans and not a passing fad. As always, if you are considering changing your diet and food habits, it's always best to do so with the support of a nutrition professional. Feel free to message me if you are considering intermittent fasting.
Logan, A. and Katzman, M. Major depressive disorder: probiotics may be an adjuvant therapy. Medical hypotheses, 64 3pp. Mattson, M. and Martin, B. BDNF and 5-HT: a dynamic duo in age-related neuronal plasticity and neurodegenerative disorders.
Trends in neurosciences, 27 10pp. Zhang, H. and Gelernter, J. Brain derived neurotrophic factor BDNF gene variants and Alzheimer's disease, affective disorders, posttraumatic stress disorder, schizophrenia, and substance dependence.
American Journal of Medical Genetics Part B: Neuropsychiatric Genetics, 4pp. Son, J. and Han, J. Neuronal autophagy and neurodegenerative diseases. Alirezaei, M. and Kiosses, W. Short-term fasting induces profound neuronal autophagy. Autophagy, 6 6pp. The views expressed in this article are those of the author.
All articles published on Nutritionist Resource are reviewed by our editorial team. I became a nutritional therapist in I specialise in mental health, but to understand diet and the brain is to understand the gut and all bodily systems - everything is connected.
For the most accurate results, please enter a full postcode. All nutrition professionals are verified. Welcome to a new year! And the year I'm hailing as "the year of no diets". Magnesium and vitamin D supplementation for anxiety is currently a hot topic in circulation on many social media pl We all know that what you eat can affect your gut and improve the appearance of your skin, but did you know that wh We use cookies to run and improve our site.
This includes cookies that are essential for the site to function as well as analytics cookies that help us understand how you use the site, security cookies to authenticate users and prevent fraud, and advertising cookies to help serve and personalise ads.
By clicking "Accept all cookies" you are giving us consent to set these cookies. All site Nutritionists Events Search. Searching for a specific Nutritionist? Try our advanced search. Nutrition and mental health.
By Maria Cross, Mental health nutritionist MSc mBANT mCNHC Published on 1st June, Updated on 27th September, How it works - BDNF BDNF is a neuroprotective substance that increases resistance to damage and encourages the growth of new neurons.
Share this article with a friend. Written by Maria Cross, Mental health nutritionist MSc mBANT mCNHC. Hythe, Kent, CT Save profile Saved. Email me. View profile.
Show comments. Find a nutritionist dealing with Nutrition and mental health What type of session are you looking for? Location Search by location. Related Articles. The year of no diets Welcome to a new year! Kacie Shoulders. Magnesium and vitamin D influences on anxiety Magnesium and vitamin D supplementation for anxiety is currently a hot topic in circulation on many social media pl Therese Conlon-Barratt.
What is nutritional psychiatry? How nutrition supports well-being We all know that what you eat can affect your gut and improve the appearance of your skin, but did you know that wh Elisabeth Carlsson.
How we use cookies We use cookies to run and improve our site. Accept all cookies Manage cookies.
: Alternate-day fasting and psychological well-being| Get the latest nutrition tips from world-leading scientists for free. | Stay in the loop via Alternate-day fasting and psychological well-being with educational materials fastin our snd. Curr Mediterranean diet and culinary traditions Rep. Increased psyychological neurotropic factor Promoting self-care in diabetes education production: As mentioned above, intermittent fasting may well-bieng BDNF production, which could have positive effects on brain function and mood. Low-carbohydrate diets LCDswhich focus on higher protein, fat, and restrictive carbohydrate composition, have become popular in recent decades To help reduce unwanted side effects, you might try out a different type of fasting or speak with a dietician or mental health professional for guidance. Prog Mol Biol Transl Sci. Effects of food deprivation on the hypothalamic feeding-regulating peptides gene expressions in serotonin depleted rats. |
| Frontiers | Fasting diets: what are the impacts on eating behaviors, sleep, mood, and well-being? | Figure Electrolyte balance support. Click here for details. Alternate-day fasting and psychological well-being, Alternate-dayy, Phelan, S, Fava, JL, Alternxte-day Wing, RR. View author publications. Nat Neurosci. In the short-term, many successful fasters report feeling better because they get the illusion of control over their appetite. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. |
| How Intermittent Fasting Affects Your Brain Health | This assessment was made using the Wilcoxon test for the analysis of quantitative variables. A total of 40 male healthcare professionals were included in the study. Their mean age was There was no statistically significant difference between their leptin, NPY, and growth hormone levels measured after and before Ramadan. In addition, no statistically significant correlation was found between their plasma ghrelin levels and phobic anxiety subscale, general severity index, and positive symptom distress index scores measured after Ramadan. However, no significant correlation was found between ghrelin levels and interpersonal sensitivity subscale scores after Ramadan. While their scale scores measured before Ramadan were positively correlated with each other, there was also a positive correlation between their scale scores measured after Ramadan. Several studies examined the effects of Ramadan fasting on mental health [ 24 , 25 , 26 ]. Yousuf and colleagues examined the effect of Ramadan fasting on depression, anxiety and stress levels in diabetic patients, including fasting patients and 50 non-fasting patients. They applied the depression anxiety stress scale DASS before and after Ramadan, and reported a statistically significant improvement in depression, anxiety and stress levels in the fasting group after Ramadan [ 24 ]. One recently published meta-analysis has suggested that Ramadan fasting is associated with improvement in stress, anxiety, and depression [ 27 ]. Erdem evaluated the effects of Ramadan fasting on a sample of 73 healthy participants by applying DASS, and reported a statistically significant decrease in their depression, anxiety, and stress scores and frequency of anxiety after Ramadan compared to those measured before Ramadan [ 28 ]. Our results are partially compatible with those in the literature. Therefore, the SDIR was applied to participants in our study. However, there was no significant difference in their SDIR scores before and after Ramadan. This result may be related to our study's small number of participants. A recent review study introduced various explanations for the differences in research results regarding the effects of fasting on mental health. Accordingly, while there was no significant change in depression, anxiety, and stress levels before and after Ramadan in individuals with initial normal mood, those with initial depression, anxiety, and stress had lower scale scores after Ramadan. As a result, Ramadan fasting may have a positive effect on individuals with depression, anxiety, and stress [ 30 ]. Ramadan fasting can affect the circadian rhythms of various biological variables, including hormones [ 2 , 31 ]. Studies have shown a competitive interaction between ghrelin and leptin in the regulation of food intake [ 17 ]. Bogdan and colleagues reported a shift in the circadian rhythm of leptin on the 23rd day of Ramadan in males who fasted during Ramadan. Still, there was no significant change in their plasma leptin levels [ 32 ]. Alzoghaibi and colleagues found no significant change in ghrelin levels during and before Ramadan fasting, and determined a significant decrease in leptin levels at 10 pm during Ramadan [ 34 ]. Studies have shown that ghrelin increases not only in response to energy deficiency, but also after exposure to stress, and have reported that prolonged fasting increases plasma ghrelin levels [ 35 ]. It has been reported that ghrelin-induced anxiolytic and antidepressant-like responses in rats on a calorie-restricted diet or administered ghrelin. Therefore, activation of the ghrelin signaling pathway in response to chronic stress may be a homeostatic adaptation that helps individuals cope with stress [ 36 ]. Another study determined that ghrelin injection caused an increase in food intake, induced anxiety, and increased memory retention in rats [ 37 ]. The results of studies on ghrelin vary. This may be because of methodological differences model, type of subject, amount of ghrelin, research method, for example. Although animal experiments shed light on potential mechanisms of ghrelin regulation of anxiety and depression, further studies are needed in humans. While there was a low degree of correlation between ghrelin levels and interpersonal sensitivity subscale scores before Ramadan, no significant correlation was found after Ramadan. Therefore, no further evaluations can be made in this regard. Our study has some strengths. In some of the previous studies, a psychiatric examination was not performed, instead, a psychiatric assessment was based on symptom severity and relevant scales. In our study, all participants were interviewed applying SCIDCV according to DSM-5, so the diagnosis of psychiatric disease was ruled out. To eliminate the possible confusing effect of BMI on the clinical results of leptin hormone produced from adipose tissue, only participants with a BMI between 19 and Blood samples were taken from all participants at am after 12 h of fasting, which was significant for the reliability of the clinical results of hormones that oscillated in a circadian pattern. These details, considered in planning the study, are the strengths of our study. Our study also has some limitations. Muslims are exposed to various life changes during Ramadan, such as mealtime, sleep—wake time, sleep duration, exposure to light, and exercise, which can affect their hormone levels [ 15 , 34 ]. Methodological differences sample selection, scales, methods used for biochemical analysis, evaluation times may have affected the study's results. The small number of participants is also a limitation of our study Additional file 1. Their plasma ghrelin levels increased after Ramadan fasting compared to those measured before Ramadan. There is a need for better-structured studies with larger samples and more variables to elucidate these mechanisms that mediate the effect of Ramadan fasting on mental health. Kartal F, Demirbay S, Mete B, Özcan C, Ünal S. The effects of Ramadan fasting on mental health in health professionals in a university hospital. Sakarya Med J. Google Scholar. Azizi F. Research in Islamic fasting and health. Ann Saudi Med. Article Google Scholar. Ghazi HA, Boughdady AM, Elsayed EBM. Effect of Ramadan fasting on physical and mental health of elderly people. World J Nurs Sci. Mattson MP, Longo VD, Harvie M. Impact of intermittent fasting on health and disease processes. Ageing Res Rev. Cherif A, Roelands B, Meeusen R, Chamari K. Effects of intermittent fasting, caloric restriction, and Ramadan intermittent fasting on cognitive performance at rest and during exercise in adults. Sports Med. Halagappa VKM, Guo Z, Pearson M, Matsuoka Y, Cutler RG, LaFerla FM, et al. Neurobil Dis. Article CAS Google Scholar. Al-Jafar R, ZografouThemeli M, Zaman S, Akbar S, Lhoste V, Khamliche A, et al. Effect of religious fasting in Ramadan on blood pressure: results from LORANS London Ramadan Study and a meta-analysis. J Am Heart Assoc. PakkirMaideen NM, Jumale A, Alatrash JI, Abdul Sukkur AA. Health benefits of Islamic intermittent fasting. J Nutr Fast Health. Varady KA, Cienfuegos S, Ezpeleta M, Gabel K. Cardiometabolic benefits of intermittent fasting. Annu Rev Nutr. Fond G, Macgregor A, Leboyer M, Michalsen A. Fasting in mood disorders: neurobiology and effectiveness. A review of the literature. Psychiatry Res. Bayani AA, Esmaeili R, Ganji G. The impact of fasting on the psychological well-being of Muslim graduate students. J Relig Health. Kazemi M, Karimi S, Ansari A, Negahban T, Hosseini S, Vazirinejad R. The effect of ramadan fasting on psychological health and depression in Sirjan Azad University students. J Rafsanjan Univ Med Sci. Moghadamnia M, Maghsoudi S. A survey of effects of fasting in Ramadan on the level of stress. J Guilan Univ Med Sci. Gilavand A, Fatahiasl J. Studying effect of fasting during Ramadan on mental health of university students in Iran: a review. J Res Med Dent Sci. Abedelmalek S, Denguezli M, Chtourou H, Souissi N, Tabka Z. Does Ramadan fasting affect acylated ghrelin and growth hormone concentrations during short-term maximal exercise in the afternoon? Biol Rhythm Res. Boroumand N, Hashemy SI. The effect of Ramadan fasting on endocrine system. J Fasting Health. Öztürk AS, Arpacı A. Med J Mustafa Kemal Univ. Fernández-Pérez L, Guerra B, Díaz-Chico JC, Flores-Morales A. Estrogens regulate the hepatic effects of growth hormone, a hormonal interplay with multiple fates. Front Endocrinol. Hartman ML, Veldhuis JD, Johnson ML, Lee MM, Alberti K, Samojlik E, et al. Augmented growth hormone GH secretory burst frequency and amplitude mediate enhanced GH secretion during a two-day fast in normal men. J Clin Endocrinol Metab. Beer S, Bircham P, Bloom S, Clark P, Hales C, Hughes C, et al. The effect of a h fast on plasma levels of pituitary, adrenal, thyroid, pancreatic and gastrointestinal hormones in healthy men and women. J Endocrinol. Derogatis L. Brief Symptom Inventory BSI , Administration, Scoring and Procedure Manual. Minneapolis, Minnesota: National Computer Systems. Inc; Sahin NH, Durak A. Brief Symptom Invetory-BSI: a study of the brief symptom inventory in Turkish youth. Turk J Psychol. Erden İmamoğlu S, Aydın B. Scale of dimensions of interpersonal relationships. Stud Psychol. Yousuf S, Syed A, Ahmedani MY. To explore the association of Ramadan fasting with symptoms of depression, anxiety, and stress in people with diabetes. Diabetes Res Clin Pract. Koushali AN, Hajiamini Z, Ebadi A, Bayat N, Khamseh F. Effect of Ramadan fasting on emotional reactions in nurses. Iran J Nurs Midwifery Res. Pourabbasi A, Shirvani MSE, Shams AH. Does Islamic fasting affect cognitive functions in adolescents? A systematic review. J Pak Med Assoc. Berthelot E, Etchecopar-Etchart D, Thellier D, Lancon C, Boyer L, Fond G. Fasting interventions for stress, anxiety and depressive symptoms: a systematic review and meta-analysis. Erdem O. The investigation of the effects of Ramadan fasting on the mood state of healthy volunteer persons. Fam Pract Palliat Care. Furuncuoglu Y, Karaca E, Aras S, Yönem A. Metabolic, biochemical and psychiatric alterations in healthy subjects during Ramadan. Pak J Nutr. Wang Y, Wu R. The effect of fasting on human metabolism and psychological health. Dis Markers. Meo SA, Hassan A. Physiological changes during fasting in Ramadan. Bogdan A, Bouchareb B, Touitou Y. Response of circulating leptin to Ramadan daytime fasting: a circadian study. Br J Nutr. Kolaczynski JW, Considine RV, Ohannesian J, Marco C, Opentanova I, Nyce MR, et al. Responses of leptin to short-term fasting and refeeding in humans: a link with ketogenesis but not ketones themselves. Alzoghaibi MA, Pandi-Perumal SR, Sharif MM, BaHammam AS. Diurnal intermittent fasting during Ramadan: the effects on leptin and ghrelin levels. PLoS ONE. Nakazato M, Murakami N, Kojima M, Matsuo H, Kangawa K, Matsukura S. A role for ghrelin in the central regulation of feeding. Lutter M, Sakata I, Osborne-Lawrence S, Rovinsky SA, Anderson JG, Jung S, et al. The orexigenic hormone ghrelin defends against depressive symptoms of chronic stress. Nat Neurosci. Carlini VP, Monzón MAE, Varas MM, Cragnolini AB, Schiöth HB, Scimonelli TN, et al. Ghrelin increases anxiety-like behavior and memory retention in rats. Biochem Biophys Res Commun. Download references. This study was supported by the Scientific Research Project Unit of The University Project No. The role of the funding body in the study was analysis of data. Department of Psychiatry, Faculty of Medicine, Malatya Turgut Ozal University, Malatya, Turkey. Department of Psychiatry, Bursa City Hospital, University of Health Sciences, Bursa, Turkey. Department of Psychiatry, Faculty of Medicine, Inonu University, Malatya, Turkey. Department of Biochemistry, Faculty of Medicine, Inonu University, Malatya, Turkey. You can also search for this author in PubMed Google Scholar. MA, participated in data collection, analysis and interpretation, literature review and writing of the study. SU, participated in the modeling, design, literature review, critical review, supervision and writing of the study. LGE, participated in conception, design, literature review, supervision and critical review of the study. MCT was involved in the material and data collection of the study. All authors read and approved the final manuscript. Correspondence to Mustafa Akan. The study was approved by Inonu University Clinical Research Ethics Committee Date-Number: Stranahan, A. Impact of energy intake and expenditure on neuronal plasticity. Baxter, L. Reduction of prefrontal cortex glucose metabolism common to three types of depression. Psychiatry 46 3 , — Drevets, W. Functional neuroimaging studies of depression: The anatomy of melancholia. Kimbrell, T. Regional cerebral glucose utilization in patients with a range of severities of unipolar depression. Balasse, E. Kinetics of ketone body metabolism in fasting humans. Sleiman, S. Exercise promotes the expression of brain derived neurotrophic factor BDNF through the action of the ketone body beta-hydroxybutyrate. Elife 5 , 1 Dias, I. Does calorie restriction improve cognition?. IBRO Rep. Laessle, R. Biological and psychological correlates of intermittent dieting behavior in young women: A model for bulimia nervosa. Polivy, J. Psychological consequences of food restriction. Dietetic Assoc. Ding, X. Effects of a 72 hours fasting on brain metabolism in healthy women studied in vivo with magnetic resonance spectroscopic imaging. Blood Flow Metab. Fried, E. Thombs, B. Somatic symptom overlap in Beck Depression Inventory—II scores following myocardial infarction. Psychiatry 1 , 61—65 Hojlund, K. Reference intervals for glucose, beta-cell polypeptides, and counterregulatory factors during prolonged fasting. Bergendahl, M. Fasting as a metabolic stress paradigm selectively amplifies cortisol secretory burst mass and delays the time of maximal nyctohemeral cortisol concentrations in healthy men. CAS PubMed Google Scholar. Galvao-Teles, A. Free cortisol in obesity; effect of fasting. Acta Endocrinol. Kelly, C. Differences and variability in plasma noradrenaline between depressive and anxiety disorders. Roy, A. Norepinephrine and its metabolites in cerebrospinal fluid, plasma, and urine: Relationship to hypothalamic-pituitary-adrenal axis function in depression. Psychiatry 45 9 , — Wyatt, R. Resting plasma catecholamine concentrations in patients with depression and anxiety. Psychiatry 24 1 , 65—70 Nowacki, J. Steroid hormone secretion after stimulation of mineralocorticoid and NMDA receptors and cardiovascular risk in patients with depression. Psychiatry 10 1 , Article CAS PubMed PubMed Central Google Scholar. Carroll, B. Cerebrospinal fluid and plasma free cortisol concentrations in depression. Beck, A. Beck depression inventory—II. Kahl, K. Altered neurometabolism in major depressive disorder: A whole brain 1 H-magnetic resonance spectroscopic imaging study at 3T. Psychiatry , Belanger, M. Brain energy metabolism: Focus on astrocyte-neuron metabolic cooperation. Cell Metab. Beer, S. The effect of a h fast on plasma levels of pituitary, adrenal, thyroid, pancreatic and gastrointestinal hormones in healthy men and women. Merl, V. Serum adiponectin concentrations during a hour fast in over- and normal-weight humans. Hu, E. Beta-hydroxybutyrate promotes the expression of BDNF in hippocampal neurons under adequate glucose supply. Neuroscience , — Ziegler, M. Relationship between norepinephrine in blood and cerebrospinal fluid in the presence of a blood-cerebrospinal fluid barrier for norepinephrine. Kawahara, Y. Long-term administration of citalopram reduces basal and stress-induced extracellular noradrenaline levels in rat brain. Psychopharmacology 1 , 73—81 Emanuele, E. Increased plasma aldosterone in patients with clinical depression. Segeda, V. Aldosterone concentrations in saliva reflect the duration and severity of depressive episode in a sex dependent manner. Hallberg, L. Decreased aldosterone in the plasma of suicide attempters with major depressive disorder. Psychiatry Res. Iob, E. Persistent depressive symptoms, HPA-axis hyperactivity, and inflammation: The role of cognitive-affective and somatic symptoms. Psychiatry 25 5 , — Duncan, L. Variation in brain-derived neurotrophic factor BDNF gene is associated with symptoms of depression. Murray, A. Novel ketone diet enhances physical and cognitive performance. FASEB J. Karege, F. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Shimizu, E. Alterations of serum levels of brain-derived neurotrophic factor BDNF in depressed patients with or without antidepressants. Yoshimura, R. Effects of paroxetine or milnacipran on serum brain-derived neurotrophic factor in depressed patients. Psychiatry 31 5 , — Lee, H. Plasma brain-derived neurotrophic factor as a peripheral marker for the action mechanism of antidepressants. Neuropsychobiology 57 4 , — Reaven, G. Obesity, insulin resistance, and cardiovascular disease. Recent Prog. Koh, K. Leptin and cardiovascular disease: Response to therapeutic interventions. Circulation 25 , — Increased epicardial adipose tissue in young adults with congenital heart disease comorbid with major depressive disorder. Effects of additional exercise training on epicardial, intra-abdominal and subcutaneous adipose tissue in major depressive disorder: A randomized pilot study. Waller, C. Blunted cortisol stress response and depression-induced hypocortisolism is related to inflammation in patients with CAD. J Am Coll Cardiol 67 9 , — Celano, C. Depression and cardiac disease: A review. Kotseva, K. Dhar, A. Depression and the link with cardiovascular disease. Van Doorn, C. Leptin resistance and hippocampal behavioral deficits. Article PubMed CAS Google Scholar. Liu, J. Adiponectin is critical in determining susceptibility to depressive behaviors and has antidepressant-like activity. Article ADS CAS PubMed PubMed Central Google Scholar. Raison, C. Cytokines sing the blues: Inflammation and the pathogenesis of depression. Trends Immunol. Reichenberg, A. Cytokine-associated emotional and cognitive disturbances in humans. Psychiatry 58 5 , — Miller, A. Cytokine targets in the brain: Impact on neurotransmitters and neurocircuits. Anxiety 30 4 , — von Elm, E. The Strengthening the Reporting of Observational Studies in Epidemiology STROBE statement: Guidelines for reporting observational studies. Lancet , — Stapel, B. In vivo magnetic resonance spectrometry imaging demonstrates comparable adaptation of brain energy metabolism to metabolic stress induced by 72 h of fasting in depressed patients and healthy volunteers. Faul, F. Methods 39 2 , — Akoglu, H. Download references. Open Access funding enabled and organized by Projekt DEAL. Funding sources had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. Department of Psychiatry, Social Psychiatry and Psychotherapy, Hannover Medical School, Carl-Neuberg-Str. Department of Cardiology and Angiology, Hannover Medical School, Hannover, Germany. Institute for Clinical Chemistry, Hannover Medical School, Hannover, Germany. Institute of Diagnostic and Interventional Neuroradiology, Hannover Medical School, Hannover, Germany. You can also search for this author in PubMed Google Scholar. Correspondence to Britta Stapel. BS, DF, MWB, JB, RL, KJ, AB, VB, SB, HF, and XQD report no conflict of interest. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Impact of fasting on stress systems and depressive symptoms in patients with major depressive disorder: a cross-sectional study. Sci Rep 12 , Download citation. Received : 15 December Accepted : 22 April Published : 10 May Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate. Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily. Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Metabolism Psychology. Abstract Major depressive disorder MDD is frequently associated with poor response to treatment. Introduction Major depressive disorder MDD is a severe mental disease predicted by the World Health Organization to be the leading cause of disease burden by 1. Results Metabolic serum parameters are comparable in the Ctrl and MDD group pre- and post-fasting Levels of glucose, insulin, triglycerides and ketones did not significantly differ in the Ctrl and MDD group at T1 Table 1. Table 1 Comparison of metabolic parameters pre- and post-fasting in Ctrl and MDD. Full size table. Figure 1. Full size image. Table 2 Comparison of metabolic parameters in MDDlow in MDDhigh pre- and post-fasting. Figure 2. Figure 3. Discussion Our study revealed similar effects of a 72 h fasting intervention on peripheral parameters of metabolism and stress systems. Effect of fasting on metabolic parameters Fasting resulted in robust metabolic changes in both study groups that are in line with previous studies in mentally healthy individuals 12 , 31 , Effect of fasting on stress systems Fasting induces metabolic stress that in turn was shown to trigger an activation of stress systems HPA axis, RAAS, sympathetic activation 20 , 21 , 22 , which were reported to be dysregulated in the context of MDD 23 , 24 , 25 , 26 , Effect of fasting on depression scores In accordance to a previous study in healthy females 17 , fasting resulted in a significant increase in BDI-2 score in the Ctrl group, while no significant effect was observed in MDD patients. Effect of fasting in MDD sub-groups based on symptom severity at the beginning of the fasting intervention Analysis of MDD sub-groups based on BDI-2 score revealed differential effects in the MDDlow and MDDhigh group in response to fasting. Conclusion This pilot study highlights a beneficial effect of fasting primarily in MDD patients that suffered from more severe symptoms and did not sufficiently respond to initial antidepressant drug treatment. Limitations This study has several limitations. Subjects and methods Subjects The present study was approved by the local ethics committee at Hannover Medical School ethics application number in accordance to the principles expressed in the Declaration of Helsinki, and all participants gave their written informed consent before entering the study. Clinical assessment and measurement of blood parameters BDI-2 score was utilized to assess depression severity References The global burden of disease. Google Scholar Hindmarch, I. Article PubMed Google Scholar Rush, A. Article PubMed Google Scholar Papakostas, G. Article PubMed PubMed Central Google Scholar Howland, R. Article Google Scholar Fuchs, E. Article CAS Google Scholar Pittenger, C. Article CAS PubMed Google Scholar Stranahan, A. Article CAS Google Scholar Baxter, L. Article CAS PubMed Google Scholar Drevets, W. Article CAS PubMed Google Scholar Kimbrell, T. Article CAS PubMed Google Scholar Balasse, E. Article CAS PubMed Google Scholar Sleiman, S. Article Google Scholar Dias, I. Article PubMed PubMed Central Google Scholar Laessle, R. Article CAS PubMed Google Scholar Polivy, J. Article CAS Google Scholar Ding, X. Article CAS PubMed Google Scholar Fried, E. Article PubMed Google Scholar Thombs, B. Article PubMed PubMed Central Google Scholar Hojlund, K. Article CAS PubMed Google Scholar Bergendahl, M. CAS PubMed Google Scholar Galvao-Teles, A. Article CAS Google Scholar Kelly, C. Article CAS PubMed Google Scholar Roy, A. Article CAS PubMed Google Scholar Wyatt, R. Article CAS PubMed Google Scholar Nowacki, J. Article CAS PubMed PubMed Central Google Scholar Carroll, B. Article CAS PubMed Google Scholar Beck, A. Article CAS PubMed Google Scholar Belanger, M. Article CAS PubMed Google Scholar Beer, S. Article CAS PubMed Google Scholar Merl, V. Article CAS Google Scholar Hu, E. Article CAS PubMed Google Scholar Ziegler, M. Article CAS PubMed Google Scholar Kawahara, Y. |
Sie sind nicht recht. Schreiben Sie mir in PM, wir werden reden.