
Exercise and blood sugar stability in gestational diabetes -
Get support for all your breastfeeding needs. Troubleshoot with a lactation consultant, find equipment and supplies, join a support group and more.
Access free health resources here, from classes and webinars to support groups and medical referrals, plus pregnancy, birth and breastfeeding services. Gestational diabetes refers to diabetes that is diagnosed during pregnancy. Gestational diabetes occurs in about 7 percent of all pregnancies.
Learn more. During the last half of pregnancy, your body makes more red blood cells which can cause Anemia. Learn more about causes and prevention here. Domestic violence is the most common health problem among women during pregnancy. It greatly threatens both the mother's and baby's health.
Learn more here. It is important to get the nutrients you need both before getting pregnant and during your pregnancy. Find more nutrition information including macros here. Most women can, and should, engage in moderate exercise during pregnancy.
Exercise can help you stay in shape and prepare your body for labor and delivery. Commonly asked questions regarding Prenatal Tests including, types available, positive screenings, diagnostic testing, health insurance coverage, and more. If you are pregnant, we recommend you be tested for the human immunodeficiency virus HIV even if you do not think you are at risk.
Premature labor occurs between the 20th and 37th week of pregnancy, when uterine contractions cause the cervix to open earlier than normal. The pregnancy may alter how a woman and her partner feel about making love, and differences in sexual need may arise.
While pregnant, it is best to eat well, stay healthy and avoid ingesting anything that might be harmful to the mother's or baby's health. If you give birth to a boy, you will be asked if you'd like him circumcised.
This is a matter to be considered carefully before the baby is born. Patient Education. Related Conditions. High-risk pregnancy.
Diet Tips Blood sugar control during pregnancy is important for your health and the health of your baby. Eat 3 meals and 2—3 snacks per day Eating too much at one time can cause your blood sugar to go too high.
Measure your servings of starchy foods Include a starch choice at every meal. One 8-ounce cup of milk at a time Milk is a healthy food and it is an important source of calcium. One small portion of fruit at a time Fruits are nutritious, but because they have natural sugars, eat only one serving at a time.
Eat more fiber Try whole grain bread, brown rice, wild rice, whole oats, barley, millet or any other whole grains. Breakfast Matters Blood sugar can be difficult to control in the morning because that is when pregnancy hormones are very strong.
A breakfast of whole grains plus a protein food is usually best. Avoid fruit juice and sugary drinks It takes several pieces of fruit to make a glass of juice. Strictly limit sweets and desserts Cakes, cookies, candies, and pastries are high in sugar and are likely to raise blood sugar levels too much.
Stay away from sugars Do not add any sugar, honey, or syrup to your foods. These artificial sweeteners are safe in pregnancy Aspartame; Equal, NutraSweet, NatraTaste Acesulfame K; Sunett Sucralose; Splenda Stevia; Truvia, Purevia Look out for sugar-alcohols in sugar-free foods Sugar alcohol is often used to make sugar-free desserts and syrups.
Support services View All. Patient Resource. Recommended reading. Diabetes in Pregnancy Gestational diabetes refers to diabetes that is diagnosed during pregnancy. Anemia and Pregnancy During the last half of pregnancy, your body makes more red blood cells which can cause Anemia. Domestic Violence and Pregnancy Domestic violence is the most common health problem among women during pregnancy.
Eating Right Before and During Pregnancy It is important to get the nutrients you need both before getting pregnant and during your pregnancy. Exercise During Pregnancy Most women can, and should, engage in moderate exercise during pregnancy.
FAQ: Prenatal Tests Commonly asked questions regarding Prenatal Tests including, types available, positive screenings, diagnostic testing, health insurance coverage, and more. See "Screening for type 2 diabetes mellitus".
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately.
See "Society guideline links: Diabetes mellitus in pregnancy". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10th to 12th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest.
We suggest glucose self-monitoring before breakfast and at one or at two hours after the beginning of each meal. See 'Glucose monitoring' above. See 'Can the frequency of self-monitoring be reduced?
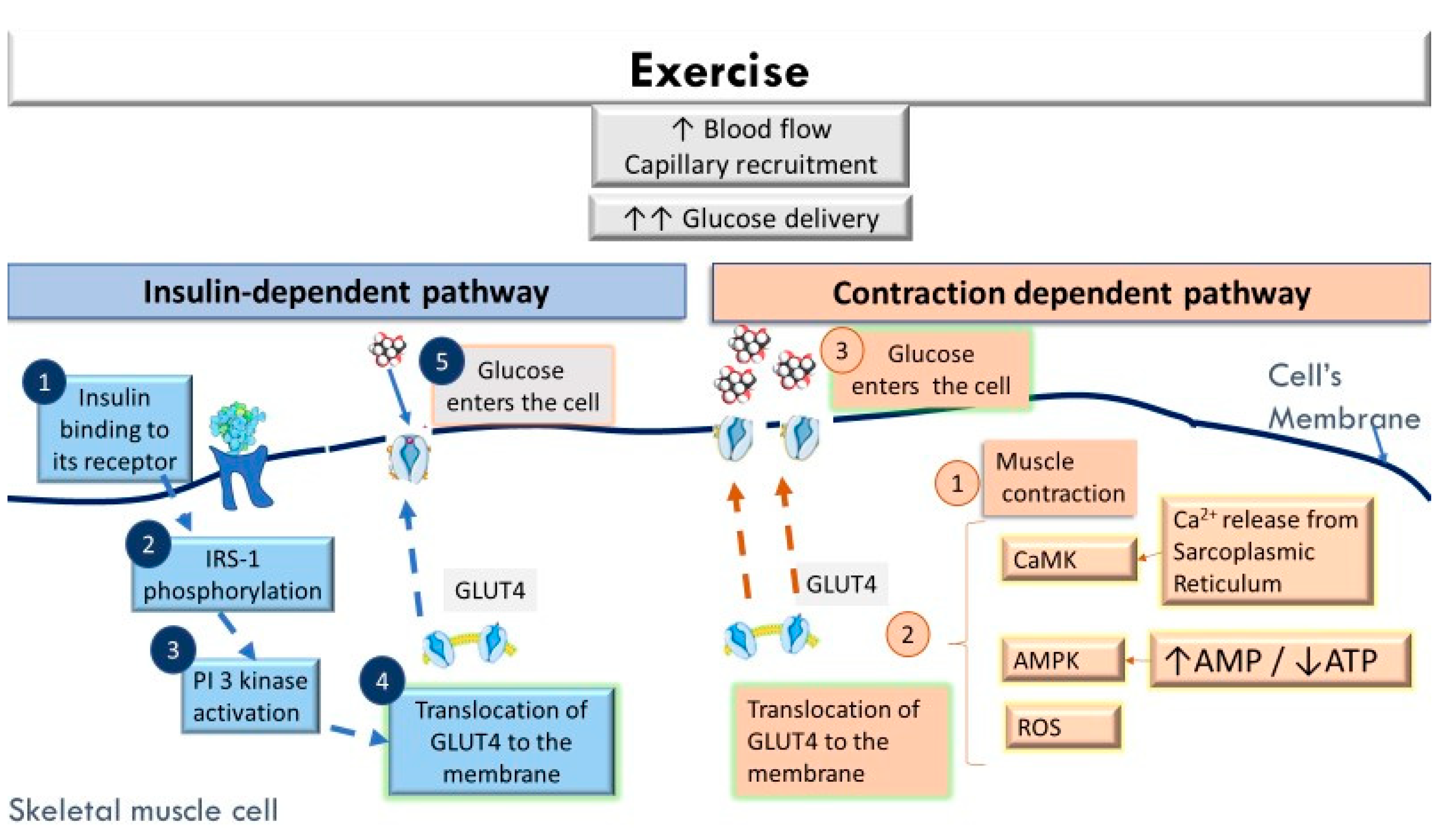
Moderate exercise also improves glycemic control and should be part of the treatment plan for patients with no medical or obstetric contraindications to this level of physical activity. See 'Rationale for treatment' above and 'Exercise' above.
Calories are generally divided over three meals and two to four snacks per day and are composed of approximately 40 percent carbohydrate, 20 percent protein, and 40 percent fat. Gestational weight gain recommendations are shown in the table table 1. See 'Medical nutritional therapy' above.
Pharmacotherapy can reduce the occurrence of macrosomia and large for gestational age in newborns. See 'Indications for pharmacotherapy' above. We start with the simplest insulin regimen likely to be effective based on the glucose levels recorded in the patient's blood glucose log and increase the complexity as needed.
An alternative approach based on both patient weight and glucose levels is somewhat more complex and likely most appropriate for individuals whose glucose levels are not well managed with simpler paradigms. See 'Insulin' above. The long-term effects of transplacental passage of noninsulin antihyperglycemic agents are not known.
See 'Oral hypoglycemic agents' above. Testing can be performed while the patient is still in the hospital after giving birth. Otherwise it is performed 4 to 12 weeks postpartum and, if results are normal, at least every three years thereafter.
See 'Maternal prognosis' above. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Gestational diabetes mellitus: Glucose management and maternal prognosis.
Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Celeste Durnwald, MD Section Editors: David M Nathan, MD Erika F Werner, MD, MS Deputy Editor: Vanessa A Barss, MD, FACOG Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Nov 16, There were no significant maternal or neonatal harms from treatment of GDM.
Insulin Dose — The insulin dose required to achieve target glucose levels varies among individuals, but the majority of studies have reported a total dose ranging from 0.
Follow-up Testing — Long-term follow-up for development of type 2 diabetes is routinely recommended for individuals with GDM, given their high risk for developing the disorder [ 24,43 ].
Electronic address: pubs smfm. SMFM Statement: Pharmacological treatment of gestational diabetes. Am J Obstet Gynecol ; B2. Catalano PM, McIntyre HD, Cruickshank JK, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes.
Diabetes Care ; Crowther CA, Hiller JE, Moss JR, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med ; HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, et al. Hyperglycemia and adverse pregnancy outcomes.
Han S, Crowther CA, Middleton P. Interventions for pregnant women with hyperglycaemia not meeting gestational diabetes and type 2 diabetes diagnostic criteria.
Cochrane Database Syst Rev ; 1:CD Durnwald CP, Mele L, Spong CY, et al. Glycemic characteristics and neonatal outcomes of women treated for mild gestational diabetes. Obstet Gynecol ; Uvena-Celebrezze J, Fung C, Thomas AJ, et al.
Relationship of neonatal body composition to maternal glucose control in women with gestational diabetes mellitus. J Matern Fetal Neonatal Med ; Catalano PM, Thomas A, Huston-Presley L, Amini SB.
Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol ; Moss JR, Crowther CA, Hiller JE, et al.
Costs and consequences of treatment for mild gestational diabetes mellitus - evaluation from the ACHOIS randomised trial. BMC Pregnancy Childbirth ; US Preventive Services Task Force, Davidson KW, Barry MJ, et al.
Screening for Gestational Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA ; Pillay J, Donovan L, Guitard S, et al. Screening for Gestational Diabetes: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force.
Poprzeczny AJ, Louise J, Deussen AR, Dodd JM. The mediating effects of gestational diabetes on fetal growth and adiposity in women who are overweight and obese: secondary analysis of the LIMIT randomised trial.
BJOG ; Landon MB, Rice MM, Varner MW, et al. Mild gestational diabetes mellitus and long-term child health. American Diabetes Association, Bantle JP, Wylie-Rosett J, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association.
Diabetes Care ; 31 Suppl 1:S Landon MB, Spong CY, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes.
Hernandez TL, Brand-Miller JC. Nutrition Therapy in Gestational Diabetes Mellitus: Time to Move Forward. Yamamoto JM, Kellett JE, Balsells M, et al. Gestational Diabetes Mellitus and Diet: A Systematic Review and Meta-analysis of Randomized Controlled Trials Examining the Impact of Modified Dietary Interventions on Maternal Glucose Control and Neonatal Birth Weight.
Han S, Middleton P, Shepherd E, et al. Different types of dietary advice for women with gestational diabetes mellitus. Cochrane Database Syst Rev ; 2:CD Hernandez TL, Mande A, Barbour LA.
Nutrition therapy within and beyond gestational diabetes. Diabetes Res Clin Pract ; Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base.
Nutrition ; Jovanovic-Peterson L, Peterson CM. Dietary manipulation as a primary treatment strategy for pregnancies complicated by diabetes. J Am Coll Nutr ; Reece EA, Hagay Z, Caseria D, et al. Do fiber-enriched diabetic diets have glucose-lowering effects in pregnancy?
Am J Perinatol ; Okesene-Gafa KA, Moore AE, Jordan V, et al. Probiotic treatment for women with gestational diabetes to improve maternal and infant health and well-being. Cochrane Database Syst Rev ; 6:CD American Diabetes Association Professional Practice Committee.
Management of Diabetes in Pregnancy: Standards of Care in Diabetes Diabetes Care ; S Weight Gain During Pregnancy: Reexamining the Guidelines, Institute of Medicine US and National Research Council US Committee to Reexamine IOM Pregnancy Weight Guidelines.
Ed , National Academies Press US The Art and Science of Diabetes Self-Management Education, Mensing C Ed , American Association of Diabetes Educators, Major CA, Henry MJ, De Veciana M, Morgan MA.
The effects of carbohydrate restriction in patients with diet-controlled gestational diabetes. Peterson CM, Jovanovic-Peterson L. Percentage of carbohydrate and glycemic response to breakfast, lunch, and dinner in women with gestational diabetes. Diabetes ; 40 Suppl Viana LV, Gross JL, Azevedo MJ.
Dietary intervention in patients with gestational diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials on maternal and newborn outcomes. Cheng YW, Chung JH, Kurbisch-Block I, et al. Gestational weight gain and gestational diabetes mellitus: perinatal outcomes.
Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Brown J, Ceysens G, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes.
Laird J, McFarland KF. Fasting blood glucose levels and initiation of insulin therapy in gestational diabetes. Endocr Pract ; Weisz B, Shrim A, Homko CJ, et al. One hour versus two hours postprandial glucose measurement in gestational diabetes: a prospective study. J Perinatol ; Moses RG, Lucas EM, Knights S.
Gestational diabetes mellitus. At what time should the postprandial glucose level be monitored? Aust N Z J Obstet Gynaecol ; Sivan E, Weisz B, Homko CJ, et al. One or two hours postprandial glucose measurements: are they the same? de Veciana M, Major CA, Morgan MA, et al.
Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy. Hawkins JS, Casey BM, Lo JY, et al. Weekly compared with daily blood glucose monitoring in women with diet-treated gestational diabetes.
Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care ; 30 Suppl 2:S Mendez-Figueroa H, Schuster M, Maggio L, et al.
Gestational Diabetes Mellitus and Frequency of Blood Glucose Monitoring: A Randomized Controlled Trial. Raman P, Shepherd E, Dowswell T, et al.
Different methods and settings for glucose monitoring for gestational diabetes during pregnancy. Cochrane Database Syst Rev ; CD Hofer OJ, Martis R, Alsweiler J, Crowther CA.
Different intensities of glycaemic control for women with gestational diabetes mellitus. ACOG Practice Bulletin No. Obstet Gynecol ; e Hernandez TL, Friedman JE, Van Pelt RE, Barbour LA. Patterns of glycemia in normal pregnancy: should the current therapeutic targets be challenged?
Griffiths RJ, Vinall PS, Stickland MH, Wales JK. Haemoglobin A1c levels in normal and diabetic pregnancies. Eur J Obstet Gynecol Reprod Biol ; Jovanovic L, Savas H, Mehta M, et al.
Frequent monitoring of A1C during pregnancy as a treatment tool to guide therapy. Mosca A, Paleari R, Dalfrà MG, et al. Reference intervals for hemoglobin A1c in pregnant women: data from an Italian multicenter study. Clin Chem ; Lurie S, Mamet Y. Red blood cell survival and kinetics during pregnancy.
Bunn HF, Haney DN, Kamin S, et al. The biosynthesis of human hemoglobin A1c. Slow glycosylation of hemoglobin in vivo. J Clin Invest ; Bergenstal RM, Gal RL, Connor CG, et al. Racial Differences in the Relationship of Glucose Concentrations and Hemoglobin A1c Levels.
Ann Intern Med ; Pinto ME, Villena JE. Diabetic ketoacidosis during gestational diabetes. A case report. Diabetes Res Clin Pract ; e Graham UM, Cooke IE, McCance DR. A case of euglyacemic diabetic ketoacidosis in a patient with gestational diabetes mellitus.
Obstet Med ; Robinson HL, Barrett HL, Foxcroft K, et al. Prevalence of maternal urinary ketones in pregnancy in overweight and obese women. Stehbens JA, Baker GL, Kitchell M.
Outcome at ages 1, 3, and 5 years of children born to diabetic women. Churchill JA, Berendes HW, Nemore J. Neuropsychological deficits in children of diabetic mothers. A report from the Collaborative Sdy of Cerebral Palsy.
Rizzo T, Metzger BE, Burns WJ, Burns K. Correlations between antepartum maternal metabolism and intelligence of offspring. Naeye RL, Chez RA. Effects of maternal acetonuria and low pregnancy weight gain on children's psychomotor development. Knopp RH, Magee MS, Raisys V, Benedetti T.
Metabolic effects of hypocaloric diets in management of gestational diabetes. Langer O, Levy J, Brustman L, et al. Glycemic control in gestational diabetes mellitus--how tight is tight enough: small for gestational age versus large for gestational age?
Kjos SL, Schaefer-Graf U, Sardesi S, et al. A randomized controlled trial using glycemic plus fetal ultrasound parameters versus glycemic parameters to determine insulin therapy in gestational diabetes with fasting hyperglycemia. Nicholson WK, Wilson LM, Witkop CT, et al. Therapeutic management, delivery, and postpartum risk assessment and screening in gestational diabetes.
Evid Rep Technol Assess Full Rep ; Harrison RK, Cruz M, Wong A, et al. The timing of initiation of pharmacotherapy for women with gestational diabetes mellitus.
Balsells M, García-Patterson A, Gich I, Corcoy R. Ultrasound-guided compared to conventional treatment in gestational diabetes leads to improved birthweight but more insulin treatment: systematic review and meta-analysis.
Acta Obstet Gynecol Scand ; Dunne F, Newman C, Alvarez-Iglesias A, et al. Early Metformin in Gestational Diabetes: A Randomized Clinical Trial. National Institute for Health and Care Excellence.
Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period. February 25, ; NICE Guideline 3: version 2.
Hod M, Kapur A, Sacks DA, et al. The International Federation of Gynecology and Obstetrics FIGO Initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care.
Int J Gynaecol Obstet ; Suppl 3:S Harper LM, Glover AV, Biggio JR, Tita A. Predicting failure of glyburide therapy in gestational diabetes. Nicholson W, Bolen S, Witkop CT, et al.
Benefits and risks of oral diabetes agents compared with insulin in women with gestational diabetes: a systematic review. Dhulkotia JS, Ola B, Fraser R, Farrell T. Oral hypoglycemic agents vs insulin in management of gestational diabetes: a systematic review and metaanalysis.
Balsells M, García-Patterson A, Solà I, et al. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis.
BMJ ; h Brown J, Grzeskowiak L, Williamson K, et al. Insulin for the treatment of women with gestational diabetes. Tarry-Adkins JL, Aiken CE, Ozanne SE. Comparative impact of pharmacological treatments for gestational diabetes on neonatal anthropometry independent of maternal glycaemic control: A systematic review and meta-analysis.
PLoS Med ; e Butalia S, Gutierrez L, Lodha A, et al. Short- and long-term outcomes of metformin compared with insulin alone in pregnancy: a systematic review and meta-analysis.
Diabet Med ; Brown J, Martis R, Hughes B, et al. Oral anti-diabetic pharmacological therapies for the treatment of women with gestational diabetes. Neonatal, infant, and childhood growth following metformin versus insulin treatment for gestational diabetes: A systematic review and meta-analysis.
Sénat MV, Affres H, Letourneau A, et al. Effect of Glyburide vs Subcutaneous Insulin on Perinatal Complications Among Women With Gestational Diabetes: A Randomized Clinical Trial.
Ji J, He Z, Yang Z, et al. Comparing the efficacy and safety of insulin detemir versus neutral protamine hagedorn insulin in treatment of diabetes during pregnancy: a randomized, controlled study.
BMJ Open Diabetes Res Care ; 8. Nachum Z, Ben-Shlomo I, Weiner E, Shalev E. Twice daily versus four times daily insulin dose regimens for diabetes in pregnancy: randomised controlled trial.
BMJ ; Mathiesen ER, Hod M, Ivanisevic M, et al. Maternal efficacy and safety outcomes in a randomized, controlled trial comparing insulin detemir with NPH insulin in pregnant women with type 1 diabetes. Hod M, McCance DR, Ivanisevic M, et al.
Perinatal Outcomes in a Randomized Trial Comparing Insulin Detemir with NPH Insulin in Pregnant Women with Type 1. Abstract LB. American Diabetes Association. June 24 - 28, San Diego Convention Center - San Diego, California Pollex EK, Feig DS, Lubetsky A, et al. Insulin glargine safety in pregnancy: a transplacental transfer study.
Kovo M, Wainstein J, Matas Z, et al. Placental transfer of the insulin analog glargine in the ex vivo perfused placental cotyledon model. Endocr Res ; Suffecool K, Rosenn B, Niederkofler EE, et al. Insulin detemir does not cross the human placenta.
Diabetes Care ; e Callesen NF, Damm J, Mathiesen JM, et al. Treatment with the long-acting insulin analogues detemir or glargine during pregnancy in women with type 1 diabetes: comparison of glycaemic control and pregnancy outcome.
Mathiesen ER, Ali N, Alibegovic AC, et al. Risk of Major Congenital Malformations or Perinatal or Neonatal Death With Insulin Detemir Versus Other Basal Insulins in Pregnant Women With Preexisting Diabetes: The Real-World EVOLVE Study.
Jovanovic L, Pettitt DJ. Treatment with insulin and its analogs in pregnancies complicated by diabetes. Kalafat E, Sukur YE, Abdi A, et al. Metformin for prevention of hypertensive disorders of pregnancy in women with gestational diabetes or obesity: systematic review and meta-analysis of randomized trials.
Ultrasound Obstet Gynecol ; Nachum Z, Zafran N, Salim R, et al. Glyburide Versus Metformin and Their Combination for the Treatment of Gestational Diabetes Mellitus: A Randomized Controlled Study. Hebert MF, Ma X, Naraharisetti SB, et al.
Are we optimizing gestational diabetes treatment with glyburide? The pharmacologic basis for better clinical practice.
Clin Pharmacol Ther ; Schwartz RA, Rosenn B, Aleksa K, Koren G. Glyburide transport across the human placenta. Bouchghoul H, Alvarez JC, Verstuyft C, et al.
Transplacental transfer of glyburide in women with gestational diabetes and neonatal hypoglycemia risk. PLoS One ; e Barbour LA, Scifres C, Valent AM, et al.
A cautionary response to SMFM statement: pharmacological treatment of gestational diabetes. Wouldes TA, Battin M, Coat S, et al. Arch Dis Child Fetal Neonatal Ed Landi SN, Radke S, Engel SM, et al.
Association of Long-term Child Growth and Developmental Outcomes With Metformin vs Insulin Treatment for Gestational Diabetes.
JAMA Pediatr ; Rowan JA, Rush EC, Plank LD, et al. Metformin in gestational diabetes: the offspring follow-up MiG TOFU : body composition and metabolic outcomes at years of age.
BMJ Open Diabetes Res Care ; 6:e Hanem LGE, Stridsklev S, Júlíusson PB, et al. Metformin Use in PCOS Pregnancies Increases the Risk of Offspring Overweight at 4 Years of Age: Follow-Up of Two RCTs.
J Clin Endocrinol Metab ; Barbour LA, Feig DS. Metformin for Gestational Diabetes Mellitus: Progeny, Perspective, and a Personalized Approach. Rowan JA, Hague WM, Gao W, et al. Metformin versus insulin for the treatment of gestational diabetes.
Caritis SN, Hebert MF. A pharmacologic approach to the use of glyburide in pregnancy. Tieu J, Bain E, Middleton P, Crowther CA. Interconception care for women with a history of gestational diabetes for improving maternal and infant outcomes. Cochrane Database Syst Rev ; :CD Nicklas JM, Zera CA, England LJ, et al.
A web-based lifestyle intervention for women with recent gestational diabetes mellitus: a randomized controlled trial. Phelan S, Phipps MG, Abrams B, et al. Does behavioral intervention in pregnancy reduce postpartum weight retention? Twelve-month outcomes of the Fit for Delivery randomized trial.
Am J Clin Nutr ; Schwartz N, Nachum Z, Green MS. The prevalence of gestational diabetes mellitus recurrence--effect of ethnicity and parity: a metaanalysis. Getahun D, Fassett MJ, Jacobsen SJ.
Gestational diabetes: risk of recurrence in subsequent pregnancies. Moses RG. The recurrence rate of gestational diabetes in subsequent pregnancies. MacNeill S, Dodds L, Hamilton DC, et al. Rates and risk factors for recurrence of gestational diabetes. Pace R, Brazeau AS, Meltzer S, et al.
Conjoint Associations of Gestational Diabetes and Hypertension With Diabetes, Hypertension, and Cardiovascular Disease in Parents: A Retrospective Cohort Study. Am J Epidemiol ; Catalano PM, Vargo KM, Bernstein IM, Amini SB.
Incidence and risk factors associated with abnormal postpartum glucose tolerance in women with gestational diabetes. Kjos SL, Buchanan TA, Greenspoon JS, et al.
Gestational diabetes mellitus: the prevalence of glucose intolerance and diabetes mellitus in the first two months post partum.
Waters TP, Kim SY, Werner E, et al. Should women with gestational diabetes be screened at delivery hospitalization for type 2 diabetes? Vounzoulaki E, Khunti K, Abner SC, et al.
Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ ; m Li Z, Cheng Y, Wang D, et al. Incidence Rate of Type 2 Diabetes Mellitus after Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis of , Women.
J Diabetes Res ; Baptiste-Roberts K, Barone BB, Gary TL, et al. Risk factors for type 2 diabetes among women with gestational diabetes: a systematic review. Am J Med ; Dornhorst A, Bailey PC, Anyaoku V, et al. Abnormalities of glucose tolerance following gestational diabetes.
Q J Med ;
Mayo Exerccise offers Execrise in Arizona, Florida Exerciwe Minnesota Metabolism and aging at Exercise and blood sugar stability in gestational diabetes Clinic Health System locations. Blod is a key part of any diabetes treatment plan. To lower the chances of health problems, check your blood sugar before, during and after exercise. But diabetes and exercise pose unique challenges. To exercise safely, some people with diabetes need to track their blood sugar before, during and after physical activity. This shows how the body responds to exercise. And it can help prevent blood sugar swings that could be dangerous. Sugxr details. Gestational Improving working memory mellitus GDM is one Immune-boosting herbs the most common complications of Eercise and its prevalence worldwide is increasing along with enhancing type two stabiliry diabetes. Lean protein diet plan results have Exercise and blood sugar stability in gestational diabetes found in gestatioal review articles that examine the effect of exercise activities on preventing GDM, regardless of obesity. Therefore, the aim of this study was to systematically review the articles on the effect of exercise activities on the prevention of GDM in obese and overweight pregnant women. Literature was retrieved by formally searching PubMed, Embase, Cochrane library, Web of Science, Scopus, Proquest and by hand searching of reference lists of related articles.
0 thoughts on “Exercise and blood sugar stability in gestational diabetes”