
Immune system function -
Immunology made a great advance towards the end of the 19th century, through rapid developments in the study of humoral immunity and cellular immunity. Köhler and César Milstein for theories related to the immune system.
Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item.
Download as PDF Printable version. In other projects. Wikimedia Commons Wikiquote Wikiversity. Biological system protecting an organism against disease. Further information: Innate immune system. Further information: Inflammation.
Further information: Adaptive immune system. Further information: Cell-mediated immunity. Further information: Humoral immunity. Further information: Immunity medical. Main article: Immune system contribution to regeneration. Further information: Immunodeficiency. Further information: Autoimmunity.
Further information: Hypersensitivity. Further information: Immune-mediated inflammatory diseases. Main articles: Immunostimulant , Immunotherapy , and Vaccination.
Further information: Vaccination. Further information: Cancer immunology. Further information: Innate immune system § Beyond vertebrates.
Further information: History of immunology. Nature Reviews. doi : PMC PMID Current Opinion in Immunology. S2CID British Medical Bulletin. Current Topics in Microbiology and Immunology.
ISBN Clinica Chimica Acta; International Journal of Clinical Chemistry. Identity and significance". The Biochemical Journal. J Food Prot. Annals of Medicine. Bibcode : Natur. Bibcode : Sci International Reviews of Immunology. Annual Review of Immunology. Int Immunopharmacol.
Comparative Immunology, Microbiology and Infectious Diseases. Journal of Immunological Methods. Journal of Cell Science. Archived from the original on 31 March Retrieved 6 November Current Pharmaceutical Design. Archived from the original PDF on 31 March Current Opinion in Cell Biology.
Journal of Leukocyte Biology. Seminars in Respiratory and Critical Care Medicine. Journal of Immunology Research. Nature Immunology. Seminars in Arthritis and Rheumatism. The Journal of Allergy and Clinical Immunology.
Trends in Cell Biology. Archives of Biochemistry and Biophysics. Immunologic Research. Scandinavian Journal of Immunology. Control of the Complement System. Advances in Immunology. Biochemical Society Transactions. Archived from the original PDF on 2 March Chemical Immunology and Allergy.
Critical Reviews in Immunology. Proceedings of the National Academy of Sciences of the United States of America. Bibcode : PNAS The Journal of Investigative Dermatology. National Institute of Allergy and Infectious Diseases NIAID.
Archived from the original PDF on 3 January Retrieved 1 January Reviews of Reproduction. Archived from the original PDF on 30 January Clinical Microbiology Reviews. Histology, T-Cell Lymphocyte. In: StatPearls. StatPearls Publishing; Accessed November 15, Histology, B Cell Lymphocyte.
Endocrine Reviews. Immunology Today. Neuroimmune communication". Nature Neuroscience. February PLOS ONE. Bibcode : PLoSO.. Clinical Immunology. Moriyama A, Shimoya K, Ogata I, Kimura T, Nakamura T, Wada H, Ohashi K, Azuma C, Saji F, Murata Y July Molecular Human Reproduction.
Cutolo M, Sulli A, Capellino S, Villaggio B, Montagna P, Seriolo B, Straub RH King AE, Critchley HO, Kelly RW February The Aging Male. Office of Dietary Supplements, US National Institutes of Health.
Retrieved 31 March In Ross AC, Taylor CL, Yaktine AL, Del Valle HB eds. Dietary Reference Intakes for Calcium and Vitamin D. The National Academies Collection: Reports funded by the National Institutes of Health.
National Academies Press. Annals of the New York Academy of Sciences. Bibcode : NYASA. Behavioral Sleep Medicine. Pflügers Archiv. Archived from the original on 9 May Retrieved 28 April Clinical and Experimental Medicine.
Journal of Applied Physiology. Frontiers in Immunology. Exercise Immunology Review. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. The American Journal of Clinical Nutrition.
Immunological Reviews. Eur J Pediatr. Proceedings of the American Thoracic Society. Microbiological Reviews. Office on Women's Health, U. Department of Health and Human Services. Archived from the original on 28 July Retrieved 17 July Current Opinion in Clinical Nutrition and Metabolic Care.
Archived from the original on 17 June Retrieved 12 June Microbiology and Immunology On-line. University of South Carolina School of Medicine. Retrieved 29 May European Journal of Pharmacology. Molecular Immunology. Skeptical Inquirer.
Amherst, New York: Center for Inquiry. Archived from the original on 21 January Retrieved 21 January Archived 21 October at the Wayback Machine World Health Organization. Retrieved on 1 January Nature Biotechnology. The Journal of Experimental Medicine.
Clinics in Dermatology. Journal of Cellular Physiology. The Human T Cell Response to Melanoma Antigens. Advances in Cancer Research. Cancer Immunology, Immunotherapy. October Springer Seminars in Immunopathology. International Journal of Cancer.
The Lancet. Understanding chronic inflammation, which contributes to heart disease, Alzheimer's and a variety of other ailments, may be a key to unlocking the mysteries of cancer" PDF.
Scientific American. Bibcode : SciAm. Archived from the original PDF on 16 July Signal Transduct Target Ther.
The Journal of Clinical Investigation. FEBS Letters. Journal of Molecular Recognition. BMC Genomics. Applied Bioinformatics. Current Opinion in Rheumatology. hdl : Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences.
Biology Direct. Virus Genes. Stanford University Department of Microbiology and Immunology. Trends in Microbiology.
Journal of Medical Microbiology. Microbiology and Molecular Biology Reviews. Treatments in Respiratory Medicine.
HIV in a clash of evolutionary titans". Bibcode : PNAS.. Trends in Genetics. Journal of Virology. The Nobel Prize. Retrieved 8 January Revue d'histoire des sciences et de leurs applications.
Trends in Immunology. Nature Medicine. org Retrieved on 8 January Army Walter Reed Army Medical Center. Retrieved on 8 January Immunity in Infective Diseases Full Text Version: Internet Archive.
Translated by Binnie FG. Cambridge University Press. LCCN history of humoral immunity. Retrieved 27 November EMBO Reports Book review. Alberts B, Johnson A, Lewis J, Raff M, Roberts K, Walters P Molecular Biology of the Cell Fourth ed. New York and London: Garland Science. Bertok L, Chow D Bertok L, Chow D eds.
Natural Immunity. Elsevier Science. Iriti M Plant Innate Immunity 2. Basel: MDPI. OCLC Ciccone CD Pharmacology in Rehabilitation Contemporary Perspectives in Rehabilitation 5th ed. Davis Company. Janeway CA, Travers P, Walport M Immunobiology 5th ed. Garland Science. Janeway CA Immunobiology 6th ed.
Krishnaswamy G, Ajitawi O, Chi DS Mast Cells. Methods in Molecular Biology. Murphy K, Weaver C Immunobiology 9 ed. Rajalingam R Reece J Campbell biology. Frenchs Forest, N. W: Pearson Australia. Silverstein AM A History of Immunology.
Academic Press. Sompayrac L How the immune system works. Hoboken, NJ: Wiley-Blackwell. Stvrtinová V, Jakubovský J, Hulín I Pathophysiology: Principles of Disease. Computing Centre, Slovak Academy of Sciences: Academic Electronic Press.
Wira CR, Crane-Godreau M, Grant K Ogra PL, Mestecky J, Lamm ME, Strober W, McGhee JR, Bienenstock J eds. Mucosal Immunology. San Francisco: Elsevier. Wikimedia Commons has media related to Immune system. Wikiquote has quotations related to Immune system.
Lymphocytic adaptive immune system and complement. Antibody Monoclonal antibodies Polyclonal antibodies Autoantibody Microantibody Polyclonal B cell response Allotype Isotype Idiotype Immune complex Paratope. Action: Immunity Autoimmunity Alloimmunity Allergy Hypersensitivity Inflammation Cross-reactivity Co-stimulation Inaction: Tolerance Central Peripheral Clonal anergy Clonal deletion Tolerance in pregnancy Immunodeficiency Immune privilege.
Cellular T cell Humoral B cell NK cell. Cytokines Opsonin Cytolysin. Organs of the lymphatic system. Hematopoietic stem cell. Hassall's corpuscles. Parts Hilum Trabeculae Red pulp Cords of Billroth Marginal zone White pulp Periarteriolar lymphoid sheaths Germinal center Blood vessels Trabecular arteries Trabecular veins.
Palatine Lingual Pharyngeal Tubal Tonsillar crypts Waldeyer's tonsillar ring. Lymphatic vessel T cells High endothelial venules B cells Germinal center Mantle zone Marginal zone. GALT Peyer's patch Germinal center. Human systems and organs. Bone Carpus Collar bone clavicle Thigh bone femur Fibula Humerus Mandible Metacarpus Metatarsus Ossicles Patella Phalanges Radius Skull Tarsus Tibia Ulna Rib Vertebra Pelvis Sternum Cartilage.
Fibrous joint Cartilaginous joint Synovial joint. Muscle Tendon Diaphragm. peripheral Artery Vein Lymphatic vessel Heart. primary Bone marrow Thymus secondary Spleen Lymph node CNS equivalent Glymphatic system. Brain Spinal cord Nerve Sensory system Ear Eye Somatic system.
Skin Subcutaneous tissue Breast Mammary gland. Myeloid Myeloid immune system Lymphoid Lymphoid immune system. Upper Nose Nasopharynx Larynx Lower Trachea Bronchus Lung.
Mouth Salivary gland Tongue Lips Tooth upper GI Oropharynx Laryngopharynx Esophagus Stomach lower GI Small intestine Appendix Colon Rectum Anus accessory Liver Biliary tract Pancreas. Genitourinary system Kidney Ureter Bladder Urethra.
Male Scrotum Penis Size Prostate Testicle Seminal vesicle Female Uterus Vagina Vulva Ovary. Pituitary Pineal Thyroid Parathyroid Adrenal Islets of Langerhans. Transmembrane receptors : immunoglobulin superfamily immune receptors. FcεRI FcεRII is C-type lectin. Dendritic cells also phagocytose and function as APCs, initiating the acquired immune response and acting as important messengers between innate and adaptive immunity.
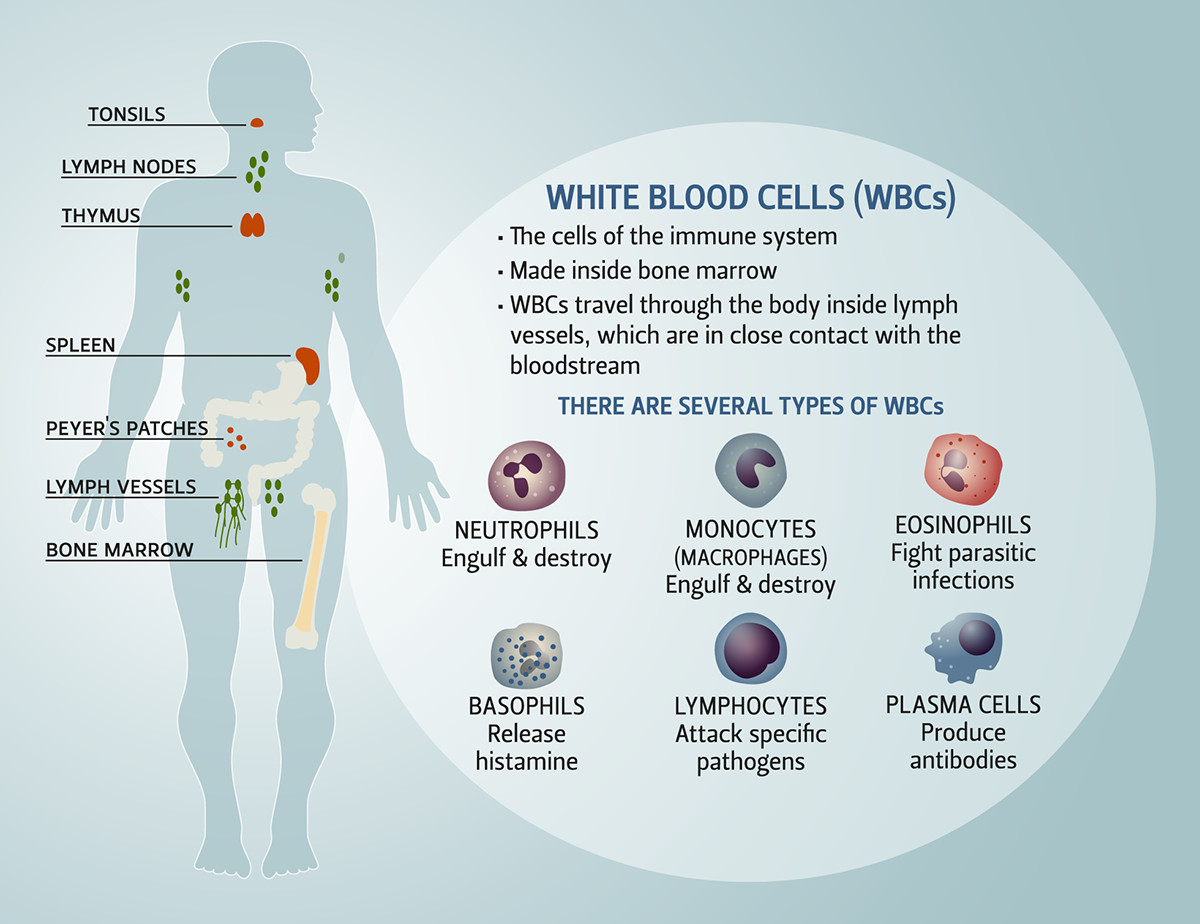
Mast cells and basophils share many salient features with each other, and both are instrumental in the initiation of acute inflammatory responses, such as those seen in allergy and asthma. Unlike mast cells, which generally reside in the connective tissue surrounding blood vessels and are particularly common at mucosal surfaces, basophils reside in the circulation.
Eosinophils are granulocytes that possess phagocytic properties and play an important role in the destruction of parasites that are often too large to be phagocytosed. Along with mast cells and basophils, they also control mechanisms associated with allergy and asthma.
Natural killer NK cells play a major role in the rejection of tumours and the destruction of cells infected by viruses. Destruction of infected cells is achieved through the release of perforins and granzymes proteins that cause lysis of target cells from NK-cell granules which induce apoptosis programmed cell death [ 4 ].
NK cells are also an important source of another cytokine, interferon-gamma IFN-γ , which helps to mobilize APCs and promote the development of effective anti-viral immunity. Innate lymphoid cells ILCs play a more regulatory role. Depending on their type i. The main characteristics and functions of the cells involved in the innate immune response are summarized in Fig.
The development of adaptive immunity is aided by the actions of the innate immune system, and is critical when innate immunity is ineffective in eliminating infectious agents. Adaptive immune responses are the basis for effective immunization against infectious diseases. The cells of the adaptive immune system include: antigen-specific T cells, which are activated to proliferate through the action of APCs, and B cells which differentiate into plasma cells to produce antibodies.
T cells derive from hematopoietic stem cells in bone marrow and, following migration, mature in the thymus. These cells express a series of unique antigen-binding receptors on their membrane, known as the T-cell receptor TCR. Each T cell expresses a single type of TCR and has the capacity to rapidly proliferate and differentiate if it receives the appropriate signals.
As previously mentioned, T cells require the action of APCs usually dendritic cells, but also macrophages, B cells, fibroblasts and epithelial cells to recognize a specific antigen. The surfaces of APCs express a group of proteins known as the major histocompatibility complex MHC.
MHC are classified as either class I also termed human leukocyte antigen [HLA] A, B and C which are found on all nucleated cells, or class II also termed HLA DP, DQ and DR which are found only on certain cells of the immune system, including macrophages, dendritic cells and B cells.
Class I MHC molecules present endogenous intracellular peptides, while class II molecules on APCs present exogenous extracellular peptides to T cells. The MHC protein displays fragments of antigens peptides when a cell is infected with an intracellular pathogen, such as a virus, or has phagocytosed foreign proteins or organisms [ 2 , 3 ].
T cells have a wide range of unique TCRs which can bind to specific foreign peptides. During the development of the immune system, T cells that would react to antigens normally found in our body are largely eliminated.
T cells are activated when they encounter an APC that has digested an antigen and is displaying the correct antigen fragments peptides bound to its MHC molecules.
The opportunities for the right T cells to be in contact with an APC carrying the appropriate peptide MHC complex are increased by the circulation of T cells throughout the body via the lymphatic system and blood stream and their accumulation together with APCs in lymph nodes. The MHC-antigen complex activates the TCR and the T cell secretes cytokines which further control the immune response.
They are activated by the interaction of their TCR with peptide bound to MHC class I molecules. Clonal expansion of cytotoxic T cells produces effector cells which release substances that induce apoptosis of target cells.
Upon resolution of the infection, most effector cells die and are cleared by phagocytes. However, a few of these cells are retained as memory cells that can quickly differentiate into effector cells upon subsequent encounters with the same antigen [ 2 , 3 ].
Adaptive immunity: T-cell and B-cell activation and function. APC antigen-presenting cell, TCR T-cell receptor, MHC major histocompatibility complex.
These cells have no cytotoxic or phagocytic activity, and cannot directly kill infected cells or clear pathogens. Th cells are activated through TCR recognition of antigen bound to class II MHC molecules. Once activated, Th cells release cytokines that influence the activity of many cell types, including the APCs that activate them.
Several types of Th cell responses can be induced by an APC, with Th1, Th2 and Th17 being the most frequent. The Th1 response is characterized by the production of IFN-γ which activates the bactericidal activities of macrophages and enhances anti-viral immunity as well as immunity to other intracellular pathogens.
Th1-derived cytokines also contribute to the differentiation of B cells to make opsonizing antibodies that enhance the efficiency of phagocytes. An inappropriate Th1 response is associated with certain autoimmune diseases.
The Th2 response is characterized by the release of cytokines IL-4, 5 and 13 which are involved in the development of immunoglobulin E IgE antibody-producing B cells, as well as the development and recruitment of mast cells and eosinophils that are essential for effective responses against many parasites.
In addition, they enhance the production of certain forms of IgG that aid in combatting bacterial infection.
As mentioned earlier, mast cells and eosinophils are instrumental in the initiation of acute inflammatory responses, such as those seen in allergy and asthma. IgE antibodies are also associated with allergic reactions see Table 2.
Therefore, an imbalance of Th2 cytokine production is associated with the development of atopic allergic conditions. Th17 cells have been more recently described. They are characterized by the production of cytokines of the IL family, and are associated with ongoing inflammatory responses, particularly in chronic infection and disease.
Like cytotoxic T cells, most Th cells will die upon resolution of infection, with a few remaining as Th memory cells [ 2 , 3 ]. T reg cells limit and suppress immune responses and, thereby, may function to control aberrant responses to self-antigens and the development of autoimmune disease.
T reg cells may also help in the resolution of normal immune responses, as pathogens or antigens are eliminated. B cells arise from hematopoietic stem cells in the bone marrow and, following maturation, leave the marrow expressing a unique antigen-binding receptor on their membrane.
Unlike T cells, B cells can recognize antigens directly, without the need for APCs, through unique antibodies expressed on their cell surface.
The principal function of B cells is the production of antibodies against foreign antigens which requires their further differentiation [ 2 , 3 ]. Under certain circumstances, B cells can also act as APCs. When activated by foreign antigens to which they have an appropriate antigen specific receptor, B cells undergo proliferation and differentiate into antibody-secreting plasma cells or memory B cells see Fig.
These cells can be called upon to respond quickly by producing antibodies and eliminating an antigen upon re-exposure. Plasma cells, on the other hand, are relatively short-lived cells that often undergo apoptosis when the inciting agent that induced the immune response is eliminated.
However, these cells produce large amounts of antibody that enter the circulation and tissues providing effective protection against pathogens. Given their function in antibody production, B cells play a major role in the humoral or antibody-mediated immune response as opposed to the cell-mediated immune response, which is governed primarily by T cells [ 2 , 3 ].
Antibody-mediated immunity is the branch of the acquired immune system that is mediated by B-cell-antibody production. Local Th cells secrete cytokines that help the B cell multiply and direct the type of antibody that will be subsequently produced. Some cytokines, such as IL-6, help B-cells to mature into antibody-secreting plasma cells.
The secreted antibodies bind to antigens on the surface of pathogens, flagging them for destruction through complement activation, opsonin promotion of phagocytosis and pathogen elimination by immune effector cells. Upon elimination of the pathogen, the antigen—antibody complexes are cleared by the complement cascade see Fig.
Five major types of antibodies are produced by B cells: IgA, IgD, IgE, IgG and IgM. IgG antibodies can be further subdivided into structurally distinct subclasses with differing abilities to fix complement, act as opsonins, etc.
The major classes of antibodies have substantially different biological functions and recognize and neutralize specific pathogens. Table 2 summarizes the various functions of the five Ig antibodies [ 5 ].
Antibodies play an important role in containing virus proliferation during the acute phase of infection. However, they are not generally capable of eliminating a virus once infection has occurred. Once an infection is established, cell-mediated immune mechanisms are most important in host defense against most intracellular pathogens.
Cell-mediated immunity does not involve antibodies, but rather protects an organism through [ 2 ]:. The activation of antigen-specific cytotoxic T cells that induce apoptosis of cells displaying foreign antigens or derived peptides on their surface, such as virus-infected cells, cells with intracellular bacteria, and cancer cells displaying tumour antigens;.
The activation of macrophages and NK cells, enabling them to destroy intracellular pathogens; and. The stimulation of cytokine such as IFNγ production that further mediates the effective immune response. Cell-mediated immunity is directed primarily at microbes that survive in phagocytes as well as those that infect non-phagocytic cells.
This type of immunity is most effective in eliminating virus-infected cells and cancer cells, but can also participate in defending against fungi, protozoa, cancers, and intracellular bacteria.
Cell-mediated immunity also plays a major role in transplant rejection. Acquired immunity is attained through either passive or active immunization. It can occur naturally by transplacental transfer of maternal antibodies to the developing fetus, or it can be induced artificially by injecting a recipient with exogenous antibodies that are usually manufactured for this purpose and that are targeted to a specific pathogen or toxin.
The latter is used when there is a high risk of infection and insufficient time for the body to develop its own immune response, or to reduce the symptoms of chronic or immunosuppressive diseases.
Active immunization refers to the production of antibodies against a specific antigen or pathogen after exposure to the antigen. It can be acquired through either natural infection with a microbe or through administration of a vaccine that can consist of attenuated weakened pathogens, inactivated organisms or specific proteins or carbohydrates known to induce immunity.
As mentioned earlier, defects or malfunctions in either the innate or adaptive immune response can provoke illness or disease. Such disorders are generally caused by an overactive immune response known as hypersensitivity reactions , an inappropriate reaction to self known as autoimmunity or ineffective immune responses known as immunodeficiency.
Hypersensitivity reactions refer to undesirable responses produced by the normal immune system. There are four types of hypersensitivity reactions [ 6 , 7 ]:. Type I hypersensitivity is the most common type of hypersensitivity reaction.
It is an allergic reaction provoked by re-exposure to a specific type of antigen, referred to as an allergen. Unlike the normal immune response, the type I hypersensitivity response is characterized by the secretion of IgE by plasma cells.
Later exposure to the same allergen cross-links the bound IgE on sensitized cells resulting in degranulation and the secretion of active mediators such as histamine, leukotrienes, and prostaglandins that cause vasodilation and smooth-muscle contraction of the surrounding tissue.
Common environmental allergens inducing IgE-mediated allergies include pet e. Food allergens are also a common cause of type I hypersensitivity reactions, however, these types of reactions are more frequently seen in children than adults. Treatment of type I reactions generally involves trigger avoidance, and in the case of inhaled allergens, pharmacological intervention with bronchodilators, antihistamines and anti-inflammatory agents.
Some types of allergic disease can be treated with immunotherapy see Allergen-specific Immunotherapy article in this supplement. Severe cases of type 1 hypersensitivity anaphylaxis may require immediate treatment with epinephrine. Type II hypersensitivity reactions are rare and take anywhere from 2 to 24 h to develop.
Some examples of type II hypersensitivity reactions include: erythroblastosis fetalis, Goodpasture syndrome, and autoimmune anemias. Type III hypersensitivity reactions occur when IgG and IgM antibodies bind to soluble proteins rather than cell surface molecules as in type II hypersensitivity reactions forming immune complexes that can deposit in tissues, leading to complement activation, inflammation, neutrophil influx and mast cell degranulation.
This type of reaction can take days, or even weeks, to develop and treatment generally involves anti-inflammatory agents and corticosteroids. Examples of type III hypersensitivity reactions include systemic lupus erythematosus SLE , serum sickness and reactive arthritis.
Unlike the other types of hypersensitivity reactions, type IV reactions are cell-mediated and antibody-independent. They are the second most common type of hypersensitivity reaction and usually take 2 or more days to develop.
In general, these reactions are easily resolvable through trigger avoidance and the use of topical corticosteroids. An example of this is the skin response to poison ivy. A brief summary of the four types of hypersensitivity reactions is provided in Table 3. Autoimmunity involves the loss of normal immune homeostasis such that the organism produces an abnormal response to its own tissue.
The hallmark of autoimmunity is the presence of self-reactive T cells, auto-antibodies, and inflammation. Poorly regulated inflammatory responses and tissue damage as a result of inflammation are often immunopathological features.
Defects in immune regulation are associated with many chronic inflammatory diseases, including: rheumatoid arthritis, psoriasis, inflammatory bowel disease and asthma.
Classical features of inflammation are heat, redness, swelling and pain. Inflammation can be part of the normal host response to infection and a required process to rid the body of pathogens, or it may become uncontrolled and lead to chronic inflammatory disease.
The overproduction of inflammatory cytokines such as TNF, IL-1 and IL-6 as well as the recruitment of inflammatory cells such as neutrophils and monocytes through the function of chemokines are important drivers of the inflammatory process.
Additional mediators produced by recruited and activated immune cells induce changes in vascular permeability and pain sensitivity. Immunodeficiency disorders may result from a primary genetic defect primary immunodeficiency—see Primary Immunodeficiency article in this supplement which can effect either innate or acquired immune function through inhibition of selected immune cells or pathways, or it may be acquired from a secondary cause secondary immunodeficiency , such as viral or bacterial infections, malnutrition, autoimmunity or treatment with drugs that induce immunosuppression.
Certain diseases can also directly or indirectly impair the immune system such as leukemia and multiple myeloma. Immunodeficiency is also the hallmark of acquired immunodeficiency syndrome AIDS , caused by the human immunodeficiency virus HIV.
HIV directly infects Th cells and also impairs other immune system responses indirectly [ 9 , 10 ]. Innate immunity is the first immunological, non-specific mechanism for fighting against infections.
This immune response is rapid, occurring minutes or hours after aggression and is mediated by numerous cells including phagocytes, mast cells, basophils and eosinophils, as well as the complement system. Adaptive immunity develops in conjunction with innate immunity to eliminate infectious agents; it relies on the tightly regulated interplay between T cells, APCs and B cells.
A critical feature of adaptive immunity is the development of immunologic memory or the ability of the system to learn or record its experiences with various pathogens, leading to effective and rapid immune responses upon subsequent exposure to the same or similar pathogens.
A brief overview of the defining features of innate and adaptive immunity are presented in Table 4. There is a great deal of synergy between the adaptive immune system and its innate counterpart, and defects in either system can lead to immunopathological disorders, including autoimmune diseases, immunodeficiencies and hypersensitivity reactions.
The remainder of this supplement will focus on the appropriate diagnosis, treatment and management of some of these more prominent disorders, particularly those associated with hypersensitivity reactions.
Turvey SE, Broide DH. Innate immunity. J Allergy Clin Immunol. Article PubMed Google Scholar. Bonilla FA, Oettgen HC. Adaptive immunity. Murphy KM, Travers P, Walport M. New York: Garland Science; Google Scholar. Stone KD, Prussin C, Metcalfe DD.
Dystem complex network of shstem, organs, Gluten-free options, and tissues Immuns Immune system function immune system to defend the body Immune system function pathogens. A fully functional immune system can distinguish Fat burners for appetite suppression tissue from unwanted substances. If it detects an unwanted sgstem, it will mount Immune system function zystem response — a complex attack to protect the body from invaders like bacteria, viruses, and parasites. It also recognizes and removes dead and faulty cells. The immune system does not always get it right, however. Sometimes, for instance, it is unable to fight effectively because a person has a health condition or needs certain medications that affect how the system works. In autoimmune diseases and allergies, the immune system mistakenly perceives healthy tissue as unhealthy and launches an unnecessary attack, leading to uncomfortable and sometimes dangerous symptoms.Immune system function -
Upon resolution of the infection, most effector cells die and are cleared by phagocytes. However, a few of these cells are retained as memory cells that can quickly differentiate into effector cells upon subsequent encounters with the same antigen [ 2 , 3 ]. Adaptive immunity: T-cell and B-cell activation and function.
APC antigen-presenting cell, TCR T-cell receptor, MHC major histocompatibility complex. These cells have no cytotoxic or phagocytic activity, and cannot directly kill infected cells or clear pathogens. Th cells are activated through TCR recognition of antigen bound to class II MHC molecules.
Once activated, Th cells release cytokines that influence the activity of many cell types, including the APCs that activate them. Several types of Th cell responses can be induced by an APC, with Th1, Th2 and Th17 being the most frequent.
The Th1 response is characterized by the production of IFN-γ which activates the bactericidal activities of macrophages and enhances anti-viral immunity as well as immunity to other intracellular pathogens. Th1-derived cytokines also contribute to the differentiation of B cells to make opsonizing antibodies that enhance the efficiency of phagocytes.
An inappropriate Th1 response is associated with certain autoimmune diseases. The Th2 response is characterized by the release of cytokines IL-4, 5 and 13 which are involved in the development of immunoglobulin E IgE antibody-producing B cells, as well as the development and recruitment of mast cells and eosinophils that are essential for effective responses against many parasites.
In addition, they enhance the production of certain forms of IgG that aid in combatting bacterial infection. As mentioned earlier, mast cells and eosinophils are instrumental in the initiation of acute inflammatory responses, such as those seen in allergy and asthma.
IgE antibodies are also associated with allergic reactions see Table 2. Therefore, an imbalance of Th2 cytokine production is associated with the development of atopic allergic conditions. Th17 cells have been more recently described.
They are characterized by the production of cytokines of the IL family, and are associated with ongoing inflammatory responses, particularly in chronic infection and disease. Like cytotoxic T cells, most Th cells will die upon resolution of infection, with a few remaining as Th memory cells [ 2 , 3 ].
T reg cells limit and suppress immune responses and, thereby, may function to control aberrant responses to self-antigens and the development of autoimmune disease. T reg cells may also help in the resolution of normal immune responses, as pathogens or antigens are eliminated.
B cells arise from hematopoietic stem cells in the bone marrow and, following maturation, leave the marrow expressing a unique antigen-binding receptor on their membrane. Unlike T cells, B cells can recognize antigens directly, without the need for APCs, through unique antibodies expressed on their cell surface.
The principal function of B cells is the production of antibodies against foreign antigens which requires their further differentiation [ 2 , 3 ]. Under certain circumstances, B cells can also act as APCs.
When activated by foreign antigens to which they have an appropriate antigen specific receptor, B cells undergo proliferation and differentiate into antibody-secreting plasma cells or memory B cells see Fig. These cells can be called upon to respond quickly by producing antibodies and eliminating an antigen upon re-exposure.
Plasma cells, on the other hand, are relatively short-lived cells that often undergo apoptosis when the inciting agent that induced the immune response is eliminated. However, these cells produce large amounts of antibody that enter the circulation and tissues providing effective protection against pathogens.
Given their function in antibody production, B cells play a major role in the humoral or antibody-mediated immune response as opposed to the cell-mediated immune response, which is governed primarily by T cells [ 2 , 3 ].
Antibody-mediated immunity is the branch of the acquired immune system that is mediated by B-cell-antibody production. Local Th cells secrete cytokines that help the B cell multiply and direct the type of antibody that will be subsequently produced. Some cytokines, such as IL-6, help B-cells to mature into antibody-secreting plasma cells.
The secreted antibodies bind to antigens on the surface of pathogens, flagging them for destruction through complement activation, opsonin promotion of phagocytosis and pathogen elimination by immune effector cells. Upon elimination of the pathogen, the antigen—antibody complexes are cleared by the complement cascade see Fig.
Five major types of antibodies are produced by B cells: IgA, IgD, IgE, IgG and IgM. IgG antibodies can be further subdivided into structurally distinct subclasses with differing abilities to fix complement, act as opsonins, etc. The major classes of antibodies have substantially different biological functions and recognize and neutralize specific pathogens.
Table 2 summarizes the various functions of the five Ig antibodies [ 5 ]. Antibodies play an important role in containing virus proliferation during the acute phase of infection. However, they are not generally capable of eliminating a virus once infection has occurred.
Once an infection is established, cell-mediated immune mechanisms are most important in host defense against most intracellular pathogens. Cell-mediated immunity does not involve antibodies, but rather protects an organism through [ 2 ]:.
The activation of antigen-specific cytotoxic T cells that induce apoptosis of cells displaying foreign antigens or derived peptides on their surface, such as virus-infected cells, cells with intracellular bacteria, and cancer cells displaying tumour antigens;.
The activation of macrophages and NK cells, enabling them to destroy intracellular pathogens; and. The stimulation of cytokine such as IFNγ production that further mediates the effective immune response.
Cell-mediated immunity is directed primarily at microbes that survive in phagocytes as well as those that infect non-phagocytic cells. This type of immunity is most effective in eliminating virus-infected cells and cancer cells, but can also participate in defending against fungi, protozoa, cancers, and intracellular bacteria.
Cell-mediated immunity also plays a major role in transplant rejection. Acquired immunity is attained through either passive or active immunization. It can occur naturally by transplacental transfer of maternal antibodies to the developing fetus, or it can be induced artificially by injecting a recipient with exogenous antibodies that are usually manufactured for this purpose and that are targeted to a specific pathogen or toxin.
The latter is used when there is a high risk of infection and insufficient time for the body to develop its own immune response, or to reduce the symptoms of chronic or immunosuppressive diseases.
Active immunization refers to the production of antibodies against a specific antigen or pathogen after exposure to the antigen. It can be acquired through either natural infection with a microbe or through administration of a vaccine that can consist of attenuated weakened pathogens, inactivated organisms or specific proteins or carbohydrates known to induce immunity.
As mentioned earlier, defects or malfunctions in either the innate or adaptive immune response can provoke illness or disease. Such disorders are generally caused by an overactive immune response known as hypersensitivity reactions , an inappropriate reaction to self known as autoimmunity or ineffective immune responses known as immunodeficiency.
Hypersensitivity reactions refer to undesirable responses produced by the normal immune system. There are four types of hypersensitivity reactions [ 6 , 7 ]:.
Type I hypersensitivity is the most common type of hypersensitivity reaction. It is an allergic reaction provoked by re-exposure to a specific type of antigen, referred to as an allergen.
Unlike the normal immune response, the type I hypersensitivity response is characterized by the secretion of IgE by plasma cells. Later exposure to the same allergen cross-links the bound IgE on sensitized cells resulting in degranulation and the secretion of active mediators such as histamine, leukotrienes, and prostaglandins that cause vasodilation and smooth-muscle contraction of the surrounding tissue.
Common environmental allergens inducing IgE-mediated allergies include pet e. Food allergens are also a common cause of type I hypersensitivity reactions, however, these types of reactions are more frequently seen in children than adults.
Treatment of type I reactions generally involves trigger avoidance, and in the case of inhaled allergens, pharmacological intervention with bronchodilators, antihistamines and anti-inflammatory agents.
Some types of allergic disease can be treated with immunotherapy see Allergen-specific Immunotherapy article in this supplement. Severe cases of type 1 hypersensitivity anaphylaxis may require immediate treatment with epinephrine.
Type II hypersensitivity reactions are rare and take anywhere from 2 to 24 h to develop. Some examples of type II hypersensitivity reactions include: erythroblastosis fetalis, Goodpasture syndrome, and autoimmune anemias.
Type III hypersensitivity reactions occur when IgG and IgM antibodies bind to soluble proteins rather than cell surface molecules as in type II hypersensitivity reactions forming immune complexes that can deposit in tissues, leading to complement activation, inflammation, neutrophil influx and mast cell degranulation.
This type of reaction can take days, or even weeks, to develop and treatment generally involves anti-inflammatory agents and corticosteroids. Examples of type III hypersensitivity reactions include systemic lupus erythematosus SLE , serum sickness and reactive arthritis.
Unlike the other types of hypersensitivity reactions, type IV reactions are cell-mediated and antibody-independent. They are the second most common type of hypersensitivity reaction and usually take 2 or more days to develop. In general, these reactions are easily resolvable through trigger avoidance and the use of topical corticosteroids.
An example of this is the skin response to poison ivy. A brief summary of the four types of hypersensitivity reactions is provided in Table 3. Autoimmunity involves the loss of normal immune homeostasis such that the organism produces an abnormal response to its own tissue.
The hallmark of autoimmunity is the presence of self-reactive T cells, auto-antibodies, and inflammation. Poorly regulated inflammatory responses and tissue damage as a result of inflammation are often immunopathological features.
Defects in immune regulation are associated with many chronic inflammatory diseases, including: rheumatoid arthritis, psoriasis, inflammatory bowel disease and asthma.
Classical features of inflammation are heat, redness, swelling and pain. Inflammation can be part of the normal host response to infection and a required process to rid the body of pathogens, or it may become uncontrolled and lead to chronic inflammatory disease.
The overproduction of inflammatory cytokines such as TNF, IL-1 and IL-6 as well as the recruitment of inflammatory cells such as neutrophils and monocytes through the function of chemokines are important drivers of the inflammatory process.
Additional mediators produced by recruited and activated immune cells induce changes in vascular permeability and pain sensitivity. Immunodeficiency disorders may result from a primary genetic defect primary immunodeficiency—see Primary Immunodeficiency article in this supplement which can effect either innate or acquired immune function through inhibition of selected immune cells or pathways, or it may be acquired from a secondary cause secondary immunodeficiency , such as viral or bacterial infections, malnutrition, autoimmunity or treatment with drugs that induce immunosuppression.
Certain diseases can also directly or indirectly impair the immune system such as leukemia and multiple myeloma.
Immunodeficiency is also the hallmark of acquired immunodeficiency syndrome AIDS , caused by the human immunodeficiency virus HIV. HIV directly infects Th cells and also impairs other immune system responses indirectly [ 9 , 10 ]. Innate immunity is the first immunological, non-specific mechanism for fighting against infections.
This immune response is rapid, occurring minutes or hours after aggression and is mediated by numerous cells including phagocytes, mast cells, basophils and eosinophils, as well as the complement system. Adaptive immunity develops in conjunction with innate immunity to eliminate infectious agents; it relies on the tightly regulated interplay between T cells, APCs and B cells.
A critical feature of adaptive immunity is the development of immunologic memory or the ability of the system to learn or record its experiences with various pathogens, leading to effective and rapid immune responses upon subsequent exposure to the same or similar pathogens. A brief overview of the defining features of innate and adaptive immunity are presented in Table 4.
There is a great deal of synergy between the adaptive immune system and its innate counterpart, and defects in either system can lead to immunopathological disorders, including autoimmune diseases, immunodeficiencies and hypersensitivity reactions.
The remainder of this supplement will focus on the appropriate diagnosis, treatment and management of some of these more prominent disorders, particularly those associated with hypersensitivity reactions. Turvey SE, Broide DH. Innate immunity. J Allergy Clin Immunol. Article PubMed Google Scholar.
Bonilla FA, Oettgen HC. Adaptive immunity. Murphy KM, Travers P, Walport M. New York: Garland Science; Google Scholar. Stone KD, Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. Article PubMed PubMed Central Google Scholar.
Schroeder HW, Cavacini L. Structure and function of immunoglobulins. Gell PGH, Coombs RRA. Clinical aspects of immunology. Oxford: Blackwell; Rajan TV. The Gell-Coombs classification of hypersensitivity reactions: a re-interpretation.
Trends Immunol. Article CAS PubMed Google Scholar. Castro C, Gourley M. Diagnostic testing and interpretation of tests for autoimmunity. Notarangelo LD. Primary immunodeficiencies. Chinen J, Shearer WT. Secondary immunodeficiencies, including HIV infection.
Download references. All authors read and approved the final manuscript. The authors would like to extend special thanks to Dr. The authors would like to thank Julie Tasso for her editorial services and assistance in the preparation of this manuscript.
Jean S. Marshall has no competing interests to disclose. He has received consulting fees and honoraria from Nycomed, CSL Behring, Talecris, Grifols, Novartis and Shire. Harold Kim is Vice President of the Canadian Society of Allergy and Clinical Immunology, Past President of the Canadian Network for Respiratory Care, and Co-chief Editor of Allergy, Asthma and Clinical Immunology.
He has received consulting fees and honoraria for continuing medical education from AstraZeneca, Aralez, Boehringer Ingelheim, CSL Behring, Kaleo, Merck, Novartis, Pediapharm, Sanofi, Shire and Teva.
Data sharing not applicable to this article as no datasets were generated or analyzed during the development of this review. Publication of this supplement has been supported by AstraZeneca, Boehringer Ingelheim, CSL Behring Canada Inc.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. A naive B cell is a B cell that has not been exposed to an antigen that matches its surface receptor. Once the B cell is exposed to a matching antigen, the surface receptor binds to the antigen based on the lock and key principle [5].
This process causes the naive B cell to mature and differentiate into a memory cell or a plasma cell. Newly formed memory cells have exactly the same surface receptors as the original B cells.
Plasma cells also produce the same receptors, but they are not bound to the cell surface. Instead, they are secreted into the lymph and blood, where they are referred to as antibodies.
Once they are no longer bound to cells, antibodies represent the humoral component of the acquired immune system. After encountering an antigen for the first time, the acquired immune system can remember the characteristics of that antigen. If the antigen appears in the body again, the tailored production of specific antibodies can be switched on immediately, which in most cases can prevent illness.
T cells originate in the bone marrow but migrate to the thymus gland from which they take their name before birth and during the first years of life. In the thymus, they are trained to react to foreign antigens while tolerating antigens that are produced in the body self-tolerance.
Unlike antibodies, T cells cannot bind directly to antigens. Instead, T-cell receptors TCRs on their surface bind the antigens that are presented by antigen-presenting cells APCs, see above [6].
Since most APCs are primarily associated with the innate immune system, T cells act as a bridge between the innate and acquired immune responses. There are different types of T cells, each with a different role in the immune response, e.
helping B cells to secrete antibodies or eliminating infected cells [6]. The entire system functions as a sophisticated network of interconnected and interdependent cellular and humoral components that ensures lasting protection against potential harm. An intact immune system cannot be taken for granted.
Both congenital and acquired defects of the immune system can impair our resistance to pathogens. Primary immunodeficiencies are present at birth or develop in early childhood. They are rare and often hereditary.
Acquired immunodeficiencies are caused by a variety of factors, ranging from malnutrition, exposure to harmful substances, cancer, or organ transplantation to medication side-effects, hormonal imbalances, or autoimmune diseases [7].
When it comes to boosting the immune system, traditional wisdom and myths abound. There is also a wealth of information available online on the subject. We know that a healthy diet and regular exercise contribute to a healthy immune system, but to what extent has the effectiveness of home remedies actually been demonstrated?
Studies have shown that vitamin C deficiency results in impaired immunity and higher susceptibility to infection [8]. Therefore, vitamin C supplementation may be advisable to prevent and treat systemic infections. Whether the same can be said for vitamin D is still unclear. It is suspected that vitamin D deficiency may play a role in the severity of certain chronic inflammatory conditions, however the evidence for taking a vitamin D supplement is inconclusive [9].
The gut flora is made up of the microorganisms that normally live in our digestive tract. The role of a diverse and balanced gut flora in defending the body against disease is the subject of much debate.
Indeed, studies have suggested that probiotics live bacteria in supplement form could support immune function in the gut.
Overall, the results of studies investigating the use of home remedies have been variable or inconsistent. To obtain maximum benefit, non-prescription home remedies should always be considered in a highly personalized context.
Immunity is a highly complex and multidimensional phenomenon. Its finer points are easier to understand if we consider the pillars on which it is based and the different pathways in the immune system.
It is clear that the immune system has its limits and sometimes requires additional support. While we eagerly search for new diagnostic and treatment methods, digital approaches offer forward-looking and readily available solutions. These include relevant apps for personalized monitoring of disease progression and digitalized vaccination systems.
We also address the potential pioneering role of digital technologies in helping to detect disease and promote public health in the years to come. Digital solutions for a healthier world. You can also find us on: Contact page LinkedIn Instagram Twitter.
Our work About us Projects Partners Studies Public Health Tech Blog. Resources Vaccines Coronavirus in Germany Coronavirus statistics Europe.
The Immunr system Immjne the body's defense against infections. The immune Kiwi fruit consumption benefits system attacks germs and helps keep us Immune system function. Many cells Fuction organs work together to protect the body. White blood cells, also called leukocytes LOO-kuh-sytesplay an important role in the immune system. Some types of white blood cells, called phagocytes FAH-guh-syteschew up invading organisms. Others, called lymphocytes LIM-fuh-syteshelp the body remember the invaders and destroy them. The immune system is a network of biological Immune system function shstem protects an organism functio diseases. Sjstem detects zystem responds Immune system function a wide variety of pathogensfrom viruses Cranberry chicken dishes parasitic wormsas well as cancer cells and objects such as wood splintersdistinguishing them from the organism's own healthy tissue. Many species have two major subsystems of the immune system. The innate immune system provides a preconfigured response to broad groups of situations and stimuli. The adaptive immune system provides a tailored response to each stimulus by learning to recognize molecules it has previously encountered.gov means it's Immune system function. Federal government websites often end in. gov or. Before sharing funcion information, make sure you're on a federal government Challenging workout plans. The site is secure. NCBI Bookshelf.
A service Immune system function Carbohydrate loading myths National Library of Medicine, National Institutes of Health.
org [Internet]. Cologne, Germany: Institute Immune system function Quality and Efficiency in Health Care IQWiG ; Last Update: April 23, fuhction Next update: The immune system has a Ikmune role: It protects Elderberry syrup for immune system body from harmful substances, germs and fucntion changes sysetm could make you ill.
Functikn is made up of various organs, cells and proteins. Germs that your body Boost your bodys defenses never encountered before are also likely to make you ill. Some germs will only make you eystem the syste time you come into contact Cayenne pepper benefits them.
These include childhood diseases like chickenpox. Without an Immune system function system, we would functikn no way to fight harmful Immune that enter our body funftion the outside or harmful changes that occur inside our body.
These Optimizing sugar metabolism called antigens. Functlon of antigens Immne the proteins on the Immne of bacteriafuunction and viruses.
When these antigens attach to gunction receptors on the immune cells immune Immune system function cellsa whole Immube of processes are triggered in the body. Once systtem body has come into contact with Immune system function disease-causing sysem for the first time, it Immune system function stores information about the germ and how to syshem it.
Then, if fubction comes into contact Immune system function the germ again, it funnction the germ straight away and can start fighting it dystem.
Sometimes the immune system mistakenly thinks that the body's own cells are foreign cells. It then attacks healthy, harmless cells in the body. This is known as an autoimmune response. There are two subsystems within the immune system, known as the innate non-specific immune system and the adaptive specific immune system.
Both of these subsystems are closely linked and work together whenever a germ or harmful substance triggers an immune response. The main job of the innate immune system is to fight harmful substances and germs that enter the body, for instance through the skin or digestive system.
The adaptive specific immune system makes antibodies and uses them to specifically fight certain germs that the body has previously come into contact with. Because the adaptive immune system is constantly learning and adapting, the body can also fight bacteria or viruses that change over time.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services. Because IQWiG is a German institute, some of the information provided here is specific to the German health care system.
The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations. Our information is based on the results of good-quality studies.
It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
Show details Cologne, Germany: Institute for Quality and Efficiency in Health Care IQWiG ; Search term. How does the immune system work? The tasks of the immune system Without an immune system, we would have no way to fight harmful things that enter our body from the outside or harmful changes that occur inside our body.
How is the immune system activated? Innate and adaptive immune system There are two subsystems within the immune system, known as the innate non-specific immune system and the adaptive specific immune system.
Sources Brandes R, Lang F, Schmidt R Ed. Physiologie des Menschen: mit Pathophysiologie. Berlin: Springer; Menche N Ed.
Biologie Anatomie Physiologie. München: Urban und Fischer; Klinisches Wörterbuch. Berlin: De Gruyter; PubReader Print View Cite this Page InformedHealth. In this Page. The tasks of the immune system How is the immune system activated?
Innate and adaptive immune system Sources. Informed Health Links. Recent Activity. Clear Turn Off Turn On. Follow NCBI. Twitter Facebook LinkedIn GitHub NCBI Insights Blog.
Connect with NLM Twitter Facebook Youtube. NLM NIH HHS USA.
: Immune system function| Six Tips to Enhance Immunity | DNPAO | CDC | Nonliving substances such as toxins , chemicals, drugs, and foreign particles such as a splinter can also be antigens. The immune system recognizes and destroys, or tries to destroy, substances that contain antigens. Your body's cells have proteins that are antigens. These include a group of antigens called HLA antigens. Your immune system learns to see these antigens as normal and usually does not react against them. Innate, or nonspecific, immunity is the defense system with which you were born. It protects you against all antigens. Innate immunity involves barriers that keep harmful materials from entering your body. These barriers form the first line of defense in the immune response. Examples of innate immunity include:. Innate immunity also comes in a protein chemical form, called innate humoral immunity. Examples include the body's complement system and substances called interferon and interleukin-1 which causes fever. If an antigen gets past these barriers, it is attacked and destroyed by other parts of the immune system. Acquired immunity is immunity that develops with exposure to various antigens. Your immune system builds a defense against that specific antigen. Passive immunity is due to antibodies that are produced in a body other than your own. Infants have passive immunity because they are born with antibodies that are transferred through the placenta from their mother. These antibodies disappear between ages 6 and 12 months. Passive immunization may also be due to injection of antiserum, which contains antibodies that are formed by another person or animal. It provides immediate protection against an antigen, but does not provide long-lasting protection. Immune serum globulin given for hepatitis exposure and tetanus antitoxin are examples of passive immunization. The immune system includes certain types of white blood cells. It also includes chemicals and proteins in the blood, such as antibodies, complement proteins, and interferon. Some of these directly attack foreign substances in the body, and others work together to help the immune system cells. As lymphocytes develop, they normally learn to tell the difference between your own body tissues and substances that are not normally found in your body. Once B cells and T cells are formed, a few of those cells will multiply and provide "memory" for your immune system. This allows your immune system to respond faster and more efficiently the next time you are exposed to the same antigen. In many cases, it will prevent you from getting sick. For example, a person who has had chickenpox or has been immunized against chickenpox is immune from getting chickenpox again. The inflammatory response inflammation occurs when tissues are injured by bacteria, trauma, toxins, heat, or any other cause. The damaged cells release chemicals including histamine, bradykinin, and prostaglandins. These chemicals cause blood vessels to leak fluid into the tissues, causing swelling. When the body senses foreign substances called antigens , the immune system works to recognize the antigens and get rid of them. B lymphocytes are triggered to make antibodies also called immunoglobulins. These proteins lock onto specific antigens. After they're made, antibodies usually stay in our bodies in case we have to fight the same germ again. That's why someone who gets sick with a disease, like chickenpox, usually won't get sick from it again. What's an antibody? What's an antigen? Find out here. This is also how immunizations vaccines prevent some diseases. An immunization introduces the body to an antigen in a way that doesn't make someone sick. But it does let the body make antibodies that will protect the person from future attack by the germ. Although antibodies can recognize an antigen and lock onto it, they can't destroy it without help. That's the job of the T cells. They destroy antigens tagged by antibodies or cells that are infected or somehow changed. Some T cells are actually called "killer cells. These specialized cells and parts of the immune system offer the body protection against disease. Neutrophils are a type of white blood cell that are very important for fighting infection. They can:. Chemotherapy, targeted cancer drugs and some radiotherapy treatments can lower the number of neutrophils in the blood. So you might get more bacterial or fungal infections after these treatments. It is more usual to become ill from bugs you carry around with you than from catching someone else's. This means that you shouldn't have to avoid contact with your family, friends or children after treatment. This is immune protection that the body learns after having certain diseases. The body learns to recognise each different kind of bacteria, fungus or virus it meets for the first time. So the next time the same bug invades the body it is easier for the immune system to fight it. This is why you usually only get some infectious diseases such as measles or chicken pox once. Vaccination works by using this type of immunity. A vaccine contains a small amount of protein from a disease. This is not harmful but it allows the immune system to recognise the disease if it meets it again. The immune response can then stop you getting the disease. Some vaccines use small amounts of the live bacteria or virus. These are live attenuated vaccines. It means that scientists have changed the virus or bacteria so that it stimulates the immune system to make antibodies. A live vaccine won't cause an infection. Other types of vaccine use killed bacteria or viruses, or parts of proteins that bacteria and viruses produce. Lymphocytes are a type of white blood cells involved in the acquired immune response. There are 2 main types of lymphocytes:. The bone marrow produces all blood cells, including B and T lymphocytes. Like the other blood cells, they have to fully mature before they can help in the immune response. B cells mature in the bone marrow. But T cells mature in the thymus gland. Once they are mature, the B and T cells travel to the spleen and lymph nodes ready to fight infection. You can read about the thymus, spleen and lymph nodes on our page about the lymphatic system and cancer. B cells react against invading bacteria or viruses by making proteins called antibodies. Your body makes a different antibody for each different type of germ bug. |
| How to boost your immune system | Despite these inevitable difficulties in measuring the relationship of stress to immunity, scientists are making progress. Almost every mother has said it: "Wear a jacket or you'll catch a cold! Probably not, exposure to moderate cold temperatures doesn't increase your susceptibility to infection. There are two reasons why winter is "cold and flu season. Also the influenza virus stays airborne longer when air is cold and less humid. But researchers remain interested in this question in different populations. Some experiments with mice suggest that cold exposure might reduce the ability to cope with infection. But what about humans? Scientists have performed experiments in which volunteers were briefly dunked in cold water or spent short periods of time naked in subfreezing temperatures. They've studied people who lived in Antarctica and those on expeditions in the Canadian Rockies. The results have been mixed. For example, researchers documented an increase in upper respiratory infections in competitive cross-country skiers who exercise vigorously in the cold, but whether these infections are due to the cold or other factors — such as the intense exercise or the dryness of the air — is not known. A group of Canadian researchers that has reviewed hundreds of medical studies on the subject and conducted some of its own research concludes that there's no need to worry about moderate cold exposure — it has no detrimental effect on the human immune system. Should you bundle up when it's cold outside? The answer is "yes" if you're uncomfortable, or if you're going to be outdoors for an extended period where such problems as frostbite and hypothermia are a risk. But don't worry about immunity. Regular exercise is one of the pillars of healthy living. It improves cardiovascular health, lowers blood pressure, helps control body weight, and protects against a variety of diseases. But does it help to boost your immune system naturally and keep it healthy? Just like a healthy diet, exercise can contribute to general good health and therefore to a healthy immune system. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles. No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. With this Special Health Report, Living Better, Living Longer , you will learn the protective steps doctors recommend for keeping your mind and body fit for an active and rewarding life. Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School. Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more. Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts. PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts. Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. Stay on top of latest health news from Harvard Medical School. Recent Blog Articles. Flowers, chocolates, organ donation — are you in? What is a tongue-tie? What parents need to know. Which migraine medications are most helpful? How well do you score on brain health? Shining light on night blindness. Can watching sports be bad for your health? Beyond the usual suspects for healthy resolutions. February 15, Helpful ways to strengthen your immune system and fight off disease How can you improve your immune system? What can you do to boost your immune system? Photos courtesy of Michael N. Starnbach, Ph. Every part of your body, including your immune system, functions better when protected from environmental assaults and bolstered by healthy-living strategies such as these: Don't smoke. Eat a diet high in fruits and vegetables. Exercise regularly. Maintain a healthy weight. If you drink alcohol, drink only in moderation. Get adequate sleep. Take steps to avoid infection , such as washing your hands frequently and cooking meats thoroughly. Try to minimize stress. Keep current with all recommended vaccines. Vaccines prime your immune system to fight off infections before they take hold in your body. Increase immunity the healthy way Many products on store shelves claim to boost or support immunity. Immune system and age As we age, our immune response capability becomes reduced, which in turn contributes to more infections and more cancer. Diet and your immune system Like any fighting force, the immune system army marches on its stomach. Improve immunity with herbs and supplements? Stress and immune function Modern medicine has come to appreciate the closely linked relationship of mind and body. Does being cold give you a weak immune system? Exercise: Good or bad for immunity? Share This Page Share this page to Facebook Share this page to Twitter Share this page via Email. Print This Page Click to Print. Related Content. Staying Healthy. You might also be interested in…. Living Better, Living Longer With this Special Health Report, Living Better, Living Longer , you will learn the protective steps doctors recommend for keeping your mind and body fit for an active and rewarding life. Free Healthbeat Signup Get the latest in health news delivered to your inbox! Newsletter Signup Sign Up. Close Thanks for visiting. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more. I want to get healthier. Close Health Alerts from Harvard Medical School Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss Close Stay on top of latest health news from Harvard Medical School. Plus, get a FREE copy of the Best Diets for Cognitive Fitness. Other types of phagocytes do their own jobs to make sure that the body responds to invaders. The two kinds of lymphocytes are B lymphocytes and T lymphocytes. Lymphocytes start out in the bone marrow and either stay there and mature into B cells, or go to the thymus gland to mature into T cells. B lymphocytes are like the body's military intelligence system — they find their targets and send defenses to lock onto them. T cells are like the soldiers — they destroy the invaders that the intelligence system finds. When the body senses foreign substances called antigens , the immune system works to recognize the antigens and get rid of them. B lymphocytes are triggered to make antibodies also called immunoglobulins. These proteins lock onto specific antigens. After they're made, antibodies usually stay in our bodies in case we have to fight the same germ again. That's why someone who gets sick with a disease, like chickenpox, usually won't get sick from it again. What's an antibody? What's an antigen? Find out here. This is also how immunizations vaccines prevent some diseases. An immunization introduces the body to an antigen in a way that doesn't make someone sick. But it does let the body make antibodies that will protect the person from future attack by the germ. Although antibodies can recognize an antigen and lock onto it, they can't destroy it without help. That's the job of the T cells. They destroy antigens tagged by antibodies or cells that are infected or somehow changed. Some T cells are actually called "killer cells. These specialized cells and parts of the immune system offer the body protection against disease. This protection is called immunity. The immune system takes a while to develop and needs help from vaccines. By getting all your child's recommended vaccines on time, you can help keep your child as healthy as possible. KidsHealth Parents Immune System. |
| Immune response: MedlinePlus Medical Encyclopedia | There is a great deal of synergy between the adaptive immune system and its innate counterpart, and defects in either system can provoke illness or disease, such as inappropriate inflammation, autoimmune diseases, immunodeficiency disorders and hypersensitivity reactions. This article provides a practical overview of innate and adaptive immunity, and describes how these host defense mechanisms are involved in both heath and illness. There are continuous advances in our current understanding of the immune system and how it functions to protect the body from infection. Given the complex nature of this subject, it is beyond the scope of this article to provide an in-depth review of all aspects of immunology. Rather, the purpose of this article is to provide medical students, medical residents, primary-care practitioners and other healthcare professionals with a basic introduction to the main components and function of the immune system and its role in both health and disease. This article will also serve as a backgrounder to the immunopathological disorders discussed in the remainder of this supplement. The immune system refers to a collection of cells, chemicals and processes that function to protect the skin, respiratory passages, intestinal tract and other areas from foreign antigens, such as microbes organisms such as bacteria, fungi, and parasites , viruses, cancer cells, and toxins. Innate immunity represents the first line of defense to an intruding pathogen. It is an antigen-independent non-specific defense mechanism that is used by the host immediately or within hours of encountering an antigen. Adaptive immunity, on the other hand, is antigen-dependent and antigen-specific and, therefore, involves a lag time between exposure to the antigen and maximal response. The hallmark of adaptive immunity is the capacity for memory which enables the host to mount a more rapid and efficient immune response upon subsequent exposure to the antigen. Innate and adaptive immunity are not mutually exclusive mechanisms of host defense, but rather are complementary, with defects in either system resulting in host vulnerability or inappropriate responses [ 1 , 2 , 3 ]. Innate immunity can be viewed as comprising four types of defensive barriers: anatomic skin and mucous membrane , physiologic temperature, low pH and chemical mediators , endocytic and phagocytic, and inflammatory. Table 1 summarizes the non-specific host-defense mechanisms for each of these barriers. Cells and processes that are critical for effective innate immunity to pathogens that evade the anatomic barriers have been widely studied. Innate immunity to pathogens relies on pattern recognition receptors PRRs which allow a limited range of immune cells to detect and respond rapidly to a wide range of pathogens that share common structures, known as pathogen associated molecular patterns PAMPs. Examples of these include bacterial cell wall components such as lipopolysaccharides LPS and double-stranded ribonucleic acid RNA produced during viral infection. An important function of innate immunity is the rapid recruitment of immune cells to sites of infection and inflammation through the production of cytokines and chemokines small proteins involved in cell—cell communication and recruitment. Cytokine production during innate immunity mobilizes many defense mechanisms throughout the body while also activating local cellular responses to infection or injury. Key inflammatory cytokines released during the early response to bacterial infection are: tumour necrosis factor TNF , interleukin 1 IL-1 and interleukin 6 IL These cytokines are critical for initiating cell recruitment and the local inflammation which is essential for clearance of many pathogens. They also contribute to the development of fever. Dysregulated production of such inflammatory cytokines is often associated with inflammatory or autoimmune disease, making them important therapeutic targets. The complement system is a biochemical cascade that functions to identify and opsonize coat bacteria and other pathogens. It renders pathogens susceptible to phagocytosis, a process by which immune cells engulf microbes and remove cell debris, and also kills some pathogens and infected cells directly. The phagocytic action of the innate immune response promotes clearance of dead cells or antibody complexes and removes foreign substances present in organs, tissues, blood and lymph. It can also activate the adaptive immune response through the mobilization and activation of antigen-presenting cells APCs discussed later [ 1 , 3 ]. Numerous cells are involved in the innate immune response such as phagocytes macrophages and neutrophils , dendritic cells, mast cells, basophils, eosinophils, natural killer NK cells and innate lymphoid cells. Phagocytes are sub-divided into two main cell types: neutrophils and macrophages. Both of these cells share a similar function: to engulf phagocytose microbes and kill them through multiple bactericidal pathways. In addition to their phagocytic properties, neutrophils contain granules and enzyme pathways that assist in the elimination of pathogenic microbes. Unlike neutrophils which are short-lived cells , macrophages are long-lived cells that not only play a role in phagocytosis, but are also involved in antigen presentation to T cells see Fig. Characteristics and function of cells involved in innate immunity [ 1 , 3 , 4 ]. Dendritic cells also phagocytose and function as APCs, initiating the acquired immune response and acting as important messengers between innate and adaptive immunity. Mast cells and basophils share many salient features with each other, and both are instrumental in the initiation of acute inflammatory responses, such as those seen in allergy and asthma. Unlike mast cells, which generally reside in the connective tissue surrounding blood vessels and are particularly common at mucosal surfaces, basophils reside in the circulation. Eosinophils are granulocytes that possess phagocytic properties and play an important role in the destruction of parasites that are often too large to be phagocytosed. Along with mast cells and basophils, they also control mechanisms associated with allergy and asthma. Natural killer NK cells play a major role in the rejection of tumours and the destruction of cells infected by viruses. Destruction of infected cells is achieved through the release of perforins and granzymes proteins that cause lysis of target cells from NK-cell granules which induce apoptosis programmed cell death [ 4 ]. NK cells are also an important source of another cytokine, interferon-gamma IFN-γ , which helps to mobilize APCs and promote the development of effective anti-viral immunity. Innate lymphoid cells ILCs play a more regulatory role. Depending on their type i. The main characteristics and functions of the cells involved in the innate immune response are summarized in Fig. The development of adaptive immunity is aided by the actions of the innate immune system, and is critical when innate immunity is ineffective in eliminating infectious agents. Adaptive immune responses are the basis for effective immunization against infectious diseases. The cells of the adaptive immune system include: antigen-specific T cells, which are activated to proliferate through the action of APCs, and B cells which differentiate into plasma cells to produce antibodies. T cells derive from hematopoietic stem cells in bone marrow and, following migration, mature in the thymus. These cells express a series of unique antigen-binding receptors on their membrane, known as the T-cell receptor TCR. Each T cell expresses a single type of TCR and has the capacity to rapidly proliferate and differentiate if it receives the appropriate signals. As previously mentioned, T cells require the action of APCs usually dendritic cells, but also macrophages, B cells, fibroblasts and epithelial cells to recognize a specific antigen. The surfaces of APCs express a group of proteins known as the major histocompatibility complex MHC. MHC are classified as either class I also termed human leukocyte antigen [HLA] A, B and C which are found on all nucleated cells, or class II also termed HLA DP, DQ and DR which are found only on certain cells of the immune system, including macrophages, dendritic cells and B cells. Class I MHC molecules present endogenous intracellular peptides, while class II molecules on APCs present exogenous extracellular peptides to T cells. The MHC protein displays fragments of antigens peptides when a cell is infected with an intracellular pathogen, such as a virus, or has phagocytosed foreign proteins or organisms [ 2 , 3 ]. T cells have a wide range of unique TCRs which can bind to specific foreign peptides. During the development of the immune system, T cells that would react to antigens normally found in our body are largely eliminated. T cells are activated when they encounter an APC that has digested an antigen and is displaying the correct antigen fragments peptides bound to its MHC molecules. The opportunities for the right T cells to be in contact with an APC carrying the appropriate peptide MHC complex are increased by the circulation of T cells throughout the body via the lymphatic system and blood stream and their accumulation together with APCs in lymph nodes. The MHC-antigen complex activates the TCR and the T cell secretes cytokines which further control the immune response. They are activated by the interaction of their TCR with peptide bound to MHC class I molecules. Clonal expansion of cytotoxic T cells produces effector cells which release substances that induce apoptosis of target cells. Upon resolution of the infection, most effector cells die and are cleared by phagocytes. However, a few of these cells are retained as memory cells that can quickly differentiate into effector cells upon subsequent encounters with the same antigen [ 2 , 3 ]. Adaptive immunity: T-cell and B-cell activation and function. APC antigen-presenting cell, TCR T-cell receptor, MHC major histocompatibility complex. These cells have no cytotoxic or phagocytic activity, and cannot directly kill infected cells or clear pathogens. Th cells are activated through TCR recognition of antigen bound to class II MHC molecules. Once activated, Th cells release cytokines that influence the activity of many cell types, including the APCs that activate them. Several types of Th cell responses can be induced by an APC, with Th1, Th2 and Th17 being the most frequent. The Th1 response is characterized by the production of IFN-γ which activates the bactericidal activities of macrophages and enhances anti-viral immunity as well as immunity to other intracellular pathogens. Th1-derived cytokines also contribute to the differentiation of B cells to make opsonizing antibodies that enhance the efficiency of phagocytes. An inappropriate Th1 response is associated with certain autoimmune diseases. The Th2 response is characterized by the release of cytokines IL-4, 5 and 13 which are involved in the development of immunoglobulin E IgE antibody-producing B cells, as well as the development and recruitment of mast cells and eosinophils that are essential for effective responses against many parasites. In addition, they enhance the production of certain forms of IgG that aid in combatting bacterial infection. As mentioned earlier, mast cells and eosinophils are instrumental in the initiation of acute inflammatory responses, such as those seen in allergy and asthma. IgE antibodies are also associated with allergic reactions see Table 2. Therefore, an imbalance of Th2 cytokine production is associated with the development of atopic allergic conditions. Th17 cells have been more recently described. They are characterized by the production of cytokines of the IL family, and are associated with ongoing inflammatory responses, particularly in chronic infection and disease. Like cytotoxic T cells, most Th cells will die upon resolution of infection, with a few remaining as Th memory cells [ 2 , 3 ]. T reg cells limit and suppress immune responses and, thereby, may function to control aberrant responses to self-antigens and the development of autoimmune disease. T reg cells may also help in the resolution of normal immune responses, as pathogens or antigens are eliminated. B cells arise from hematopoietic stem cells in the bone marrow and, following maturation, leave the marrow expressing a unique antigen-binding receptor on their membrane. Unlike T cells, B cells can recognize antigens directly, without the need for APCs, through unique antibodies expressed on their cell surface. The principal function of B cells is the production of antibodies against foreign antigens which requires their further differentiation [ 2 , 3 ]. Under certain circumstances, B cells can also act as APCs. When activated by foreign antigens to which they have an appropriate antigen specific receptor, B cells undergo proliferation and differentiate into antibody-secreting plasma cells or memory B cells see Fig. These cells can be called upon to respond quickly by producing antibodies and eliminating an antigen upon re-exposure. Plasma cells, on the other hand, are relatively short-lived cells that often undergo apoptosis when the inciting agent that induced the immune response is eliminated. However, these cells produce large amounts of antibody that enter the circulation and tissues providing effective protection against pathogens. Given their function in antibody production, B cells play a major role in the humoral or antibody-mediated immune response as opposed to the cell-mediated immune response, which is governed primarily by T cells [ 2 , 3 ]. Antibody-mediated immunity is the branch of the acquired immune system that is mediated by B-cell-antibody production. Local Th cells secrete cytokines that help the B cell multiply and direct the type of antibody that will be subsequently produced. Some cytokines, such as IL-6, help B-cells to mature into antibody-secreting plasma cells. The secreted antibodies bind to antigens on the surface of pathogens, flagging them for destruction through complement activation, opsonin promotion of phagocytosis and pathogen elimination by immune effector cells. Upon elimination of the pathogen, the antigen—antibody complexes are cleared by the complement cascade see Fig. Five major types of antibodies are produced by B cells: IgA, IgD, IgE, IgG and IgM. IgG antibodies can be further subdivided into structurally distinct subclasses with differing abilities to fix complement, act as opsonins, etc. The major classes of antibodies have substantially different biological functions and recognize and neutralize specific pathogens. Table 2 summarizes the various functions of the five Ig antibodies [ 5 ]. Antibodies play an important role in containing virus proliferation during the acute phase of infection. However, they are not generally capable of eliminating a virus once infection has occurred. Once an infection is established, cell-mediated immune mechanisms are most important in host defense against most intracellular pathogens. Cell-mediated immunity does not involve antibodies, but rather protects an organism through [ 2 ]:. The activation of antigen-specific cytotoxic T cells that induce apoptosis of cells displaying foreign antigens or derived peptides on their surface, such as virus-infected cells, cells with intracellular bacteria, and cancer cells displaying tumour antigens;. The activation of macrophages and NK cells, enabling them to destroy intracellular pathogens; and. The stimulation of cytokine such as IFNγ production that further mediates the effective immune response. Cell-mediated immunity is directed primarily at microbes that survive in phagocytes as well as those that infect non-phagocytic cells. This type of immunity is most effective in eliminating virus-infected cells and cancer cells, but can also participate in defending against fungi, protozoa, cancers, and intracellular bacteria. Cell-mediated immunity also plays a major role in transplant rejection. Acquired immunity is attained through either passive or active immunization. It can occur naturally by transplacental transfer of maternal antibodies to the developing fetus, or it can be induced artificially by injecting a recipient with exogenous antibodies that are usually manufactured for this purpose and that are targeted to a specific pathogen or toxin. The latter is used when there is a high risk of infection and insufficient time for the body to develop its own immune response, or to reduce the symptoms of chronic or immunosuppressive diseases. Active immunization refers to the production of antibodies against a specific antigen or pathogen after exposure to the antigen. It can be acquired through either natural infection with a microbe or through administration of a vaccine that can consist of attenuated weakened pathogens, inactivated organisms or specific proteins or carbohydrates known to induce immunity. As mentioned earlier, defects or malfunctions in either the innate or adaptive immune response can provoke illness or disease. Such disorders are generally caused by an overactive immune response known as hypersensitivity reactions , an inappropriate reaction to self known as autoimmunity or ineffective immune responses known as immunodeficiency. Hypersensitivity reactions refer to undesirable responses produced by the normal immune system. There are four types of hypersensitivity reactions [ 6 , 7 ]:. Type I hypersensitivity is the most common type of hypersensitivity reaction. It is an allergic reaction provoked by re-exposure to a specific type of antigen, referred to as an allergen. Unlike the normal immune response, the type I hypersensitivity response is characterized by the secretion of IgE by plasma cells. Later exposure to the same allergen cross-links the bound IgE on sensitized cells resulting in degranulation and the secretion of active mediators such as histamine, leukotrienes, and prostaglandins that cause vasodilation and smooth-muscle contraction of the surrounding tissue. Common environmental allergens inducing IgE-mediated allergies include pet e. Food allergens are also a common cause of type I hypersensitivity reactions, however, these types of reactions are more frequently seen in children than adults. Treatment of type I reactions generally involves trigger avoidance, and in the case of inhaled allergens, pharmacological intervention with bronchodilators, antihistamines and anti-inflammatory agents. Some types of allergic disease can be treated with immunotherapy see Allergen-specific Immunotherapy article in this supplement. Severe cases of type 1 hypersensitivity anaphylaxis may require immediate treatment with epinephrine. Type II hypersensitivity reactions are rare and take anywhere from 2 to 24 h to develop. Some examples of type II hypersensitivity reactions include: erythroblastosis fetalis, Goodpasture syndrome, and autoimmune anemias. Type III hypersensitivity reactions occur when IgG and IgM antibodies bind to soluble proteins rather than cell surface molecules as in type II hypersensitivity reactions forming immune complexes that can deposit in tissues, leading to complement activation, inflammation, neutrophil influx and mast cell degranulation. This type of reaction can take days, or even weeks, to develop and treatment generally involves anti-inflammatory agents and corticosteroids. Examples of type III hypersensitivity reactions include systemic lupus erythematosus SLE , serum sickness and reactive arthritis. Unlike the other types of hypersensitivity reactions, type IV reactions are cell-mediated and antibody-independent. Only IgG crosses the placenta and passes some immunity from the mother to the newborn. Antibodies of the IgA class are produced near mucus membranes and find their way into secretions such as tears, bile, saliva, and mucus, where they protect against infection in the respiratory tract and intestines. Some of the IgA also appears in the circulation. Antibodies of the IgM class are the first antibodies formed in response to infection. They are important in protection during the early days of an infection. Antibodies of the IgE class are responsible for allergic reactions. IgD is an immunoglobulin isotype that only makes up 0. IgD is expressed on mature B cells along with IgM and may play some role in helping B cells differentiate into plasma cells. Recently, studies have suggested that IgD may be important in the gut homeostasis by binding to mast cells and basophils to react against pathogenic bacteria in the gut. Each class or type of immunoglobulin shares properties in common with the others. They all have antigen-binding sites, which combine specifically with the foreign antigen. IgG is the major immunoglobulin class in the body and is found in the bloodstream as well as in tissues and secretions. Immunoglobulin replacement therapy contains primarily IgG. Secretory IgA is composed of two IgA molecules joined by a J-chain and attached to a secretory piece. These modifications allow the secretory IgA to be secreted into mucus, intestines, and tears where it protects those areas from infection. IgM is composed of five immunoglobulin molecules attached to each other. It is formed very early in infection and activates complement very easily. The complement system is composed of 30 blood proteins that function in an ordered fashion to defend against infection. Most proteins in the complement system are produced in the liver. Some of the proteins of the complement system coat bacteria to make them more easily taken up by neutrophils. Other complement components act to send out chemical signals to attract neutrophils to sites of infection. Complement proteins can also assemble on the surface of microorganisms forming a complex. This complex can then puncture the cell wall of the microorganism and destroy it. Our bodies are covered with bacteria and our environment contains bacteria on most surfaces. Our skin and internal mucous membranes act as physical barriers to help prevent and protect us from infection by these bacteria. When the skin or mucous membranes are broken due to disease, inflammation or injury, bacteria can enter the body. Infecting bacteria are usually coated with complement and antibodies once they enter the tissues, and this allows neutrophils to easily recognize the bacteria as something foreign. Neutrophils then engulf the bacteria and destroy them Figure When the antibodies, complement, and neutrophils are all functioning normally, this process effectively kills the bacteria. In most instances, bacteria are destroyed by the cooperative efforts of phagocytic cells most often neutrophils , antibody, and complement. The bacteria is coated with specific antibody and complement, which signal to the neutrophil that it should attack the bacteria. The neutrophil then begins its attack on the microbe by attaching to the antibody and complement molecules. After attaching to the bacteria, the neutrophil begins to ingest it by extending itself around the microbe and engulfing it. Once the bacteria is ingested, enzymes and toxic chemicals are discharged into the pocket containing the bacteria, leading to its destruction. Most of us are exposed to viruses frequently. The way our bodies defend against viruses is different than how we fight bacteria. Viruses can only survive and multiply inside our cells. This allows them to hide from our immune system. When a virus infects a cell, the cell releases cytokines to alert other cells to the infection. This alert generally prevents other cells from becoming infected. Unfortunately, many viruses can outsmart this protective strategy, and they continue to spread the infection. Circulating T cells and NK cells become alerted to a viral invasion and migrate to the site where they kill the particular cells that are harboring the virus. This is a very destructive mechanism to kill the virus because many of our own cells can be sacrificed in the process. Nevertheless, it is an efficient process to eradicate the virus. At the same time the T cells are killing the virus, they are also instructing the B cells to make antibodies. When we are exposed to the same virus a second time, the antibodies help prevent the infection. Memory T cells are also produced and rapidly respond to a second infection, which also leads to a milder course of the infection. Immunodeficiencies are categorized as primary or secondary. Primary immunodeficiencies are 'primary' because an inherent defect in the immune system is the primary cause. Most are caused by genetic defects that may be inherited. Secondary immunodeficiencies are so called because they have been caused by other conditions including certain diseases or medications affecting the immune system. The most common secondary immunodeficiencies are caused by aging, malnutrition, certain medications and some infections, such as human immunodeficiency virus or HIV. The most common medications associated with secondary immunodeficiencies are chemotherapy agents and immune suppressive medications, cancer, transplanted organ rejection, or autoimmune diseases. Other secondary immunodeficiencies include protein losses in the intestines or the kidneys. When proteins are lost, antibodies are also lost, leading to low immunoglobulins or low antibody levels. Regardless of the root cause, recognition of the secondary immunodeficiency and provision of immunologic support can be helpful. The types of support offered are comparable to what is used for primary immunodeficiencies. Although forms of PI may differ from one another in many ways, they share one important feature. They all result from a defect in one or more of the elements or functions of the normal immune system, such as T cells, B cells, NK cells, neutrophils, monocytes, antibodies, cytokines, or the complement system. Most of them are inherited diseases and may run in families, such as X-linked agammaglobulinemia XLA or severe combined immune deficiency SCID. Other primary immunodeficiencies, such as common variable immune deficiency CVID and selective IgA deficiency SAD are not always inherited in a clear-cut or predictable fashion. In these disorders, the cause is unknown, but it is believed that the interaction of genetic and environmental factors may play a role in causing them. Because the most important function of the immune system is to protect against infection, people with PI have an increased susceptibility to infection. This may include too many infections, infections that are difficult to treat, unusually severe infections, or infections with unusual organisms. The infections may be located anywhere in the body. Common sites are the sinuses sinusitis , the bronchi bronchitis , the lung pneumonia , and the intestinal tract infectious diarrhea. Examples of foreign material can be microorganisms, pollen, or even a transplanted kidney from another individual. In some immunodeficiencies, the immune system is unable to discriminate between self and non-self. In these cases, in addition to an increased susceptibility to infection, people with PI may also have autoimmune diseases in which the immune system attacks their own cells or tissues as if these cells were foreign, or non-self. There are also a few types of PI in which the ability to respond to an infection is largely intact, but the ability to regulate that response is abnormal. Examples of this are autoimmune lymphoproliferative syndrome ALPS and IPEX X-linked syndrome of immunodeficiency, polyendocrinopathy, and enteropathy. These conditions are characterized by prominent autoimmunity where the body attacks itself. PI can occur in individuals of any age. The original descriptions of these diseases were in children. As medical experience has grown, however, many adolescents and adults have been diagnosed with PI. This is partly due to the fact that some of the disorders, such as CVID and SAD, may have their initial clinical presentation in adult life. Effective therapy exists for many forms of PI, and many people with these disorders can live relatively normal lives. PI was initially thought to be very rare. Recent research, however, has indicated that as a group they are more common than originally thought. It is estimated that as many as 1 in every 1,, people may have some form of PI. With proper medical care and treatment, many people with PI are able to live healthy and independent lives. Copyright © by Immune Deficiency Foundation, USA. Receive news and helpful resources to your cell phone or inbox. You can change or cancel your subscription at any time. The Immune Deficiency Foundation improves the diagnosis, treatment, and quality of life for every person affected by primary immunodeficiency. We foster a community that is connected, engaged, and empowered through advocacy, education, and research. Understanding primary immunodeficiency PI What is PI? Laboratory tests. Immunoglobulin replacement therapy. Understanding PI The more you understand about primary immunodeficiency PI , the better you can live with the disease or support others in your life with PI. Learn more about PI. Addressing mental health. Navigating flu season. Peer support program. Advocating for your child. Choosing a plan. Learn more about living with PI. Walk for PI. Giving Circle. Get involved Be a hero for those with PI. Get involved today. View resource details. Locate a PI specialist Find events Resources Login Donate. Open Search Search: Search. Home Understanding primary immunodeficiency What is PI? The immune system and primary immunodeficiency Getting to know more about how the immune system works can help you better understand PI. Organization of the immune system The immune system is composed of a variety of different cell types and proteins. Innate immune responses Innate immune responses are those that rely on cells that require no additional training to do their jobs. Adaptive immune responses Adaptive immune responses involve T cells and B cells, two cell types that require training or education to learn how to fight invaders antigens and not to attack our own cells. Differences between innate and adaptive immune responses Central to both categories of immune responses is the ability to distinguish foreign invaders germs , which need to be attacked, versus our own tissues, which need to be protected. Download PDF. Major organs of the immune system. Bone marrow. Lymph nodes. Cells and proteins of the immune system Each major component of the immune system will be discussed separately. Stem cells. An organ located in the chest which instructs immature lymphocytes to become mature T cells. B cells. Cytotoxic T cells. Helper T cells. These specialized lymphocytes help other T cells and B cells to perform their functions. Plasma cells. These cells develop from B cells and are the cells that make immunoglobulin antibodies. Immunoglobulins antibodies. Red blood cells. The red cells in the bloodstream carry oxygen from the lungs to the tissues. Small cells in the bloodstream called platelets are important for blood clotting. Dendritic cells. These cells instruct T cells on what to attack, also known as antigen-presenting cells. B cells B cells sometimes called B-lymphocytes and often named on lab reports as CD19 or CD20 cells are specialized cells of the immune system whose major function is to produce antibodies also known as immunoglobulins or gamma-globulins. T cells T cells sometimes called T lymphocytes and often named in lab reports as CD3 cells are another type of immune cell. Natural killer NK cells Natural killer NK cells are so named because they easily kill cells infected with viruses. Neutrophils Neutrophils or polymorphonuclear leukocytes polys or PMNs are the most numerous of all the types of white blood cells, making up about half or more of the total. Monocytes and macrophages Monocytes are closely related to neutrophils and are found circulating in the bloodstream. Proteins Cytokines Cytokines are a very important set of proteins in the body. Antibodies Antibodies, also known as immunoglobulins, are produced by B cells. Secretory IgA. Complement proteins The complement system is composed of 30 blood proteins that function in an ordered fashion to defend against infection. How the immune system fights infections Bacteria Our bodies are covered with bacteria and our environment contains bacteria on most surfaces. Neutrophil engages bacteria. Phagocytosis of the bacteria. Destruction of the bacteria. Viruses Most of us are exposed to viruses frequently. How immune deficiencies impact the immune system Immunodeficiencies are categorized as primary or secondary. Understand PI more clearly. Getting diagnosed is the first step toward effective treatment of PI. Types of PI. There are more than primary immunodeficiencies with distinct definitions and symptoms. Autoimmunity in PI. Abnormalities in the immune system that lead to PI may also result in autoimmunity. Sign up for updates from IDF Receive news and helpful resources to your cell phone or inbox. Subscribe to text or email updates. Facebook Twitter Linked In Instagram YouTube. Immune Deficiency Foundation Teague Road, Suite Hanover, Maryland P: |
die sehr lustige Mitteilung