Glycogen storage disease type -
Early diagnosis and effective treatment can result in normal growth and puberty and many affected individuals live into adulthood and enjoy normal life activities. Many female patients have had successful pregnancies and childbirth. Type I glycogen storage disease is associated with abnormalities in two genes.
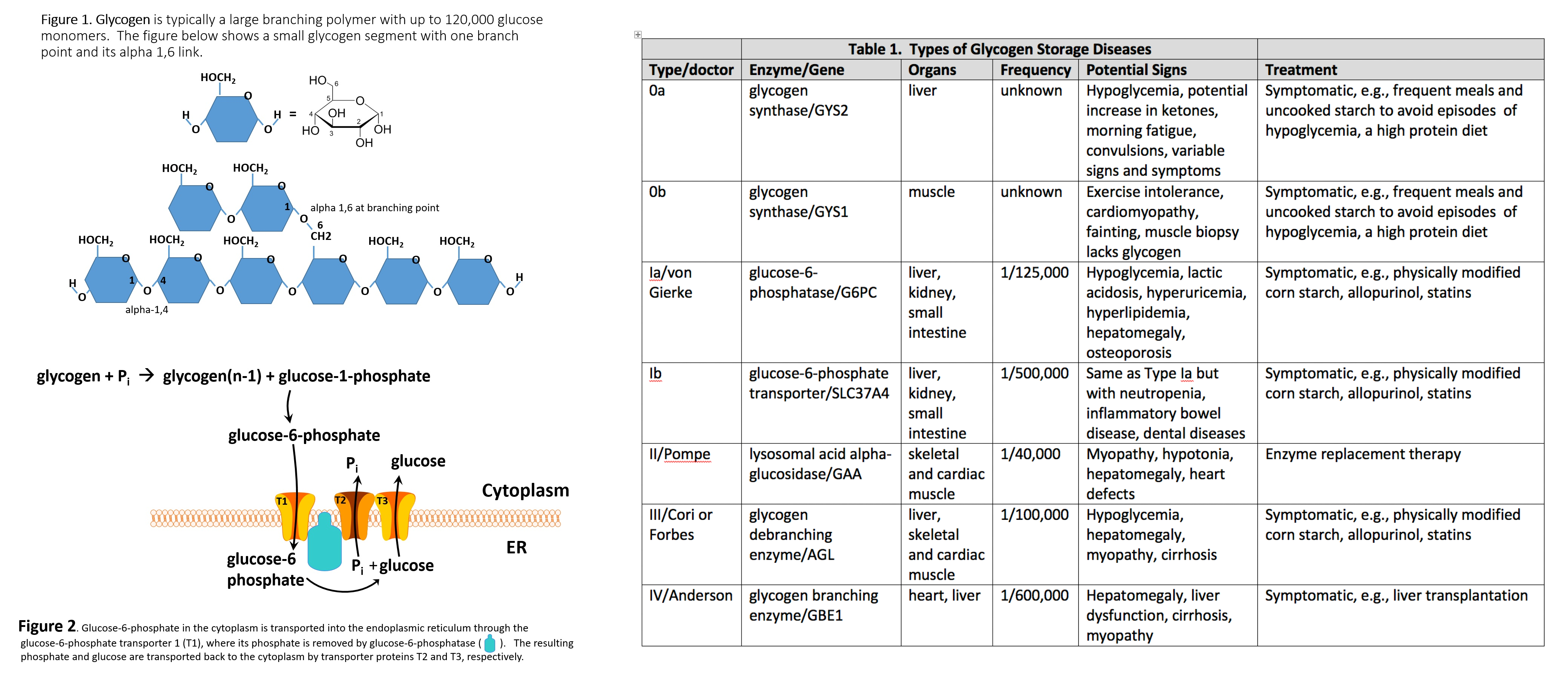
This type of GSDI is termed glycogen storage disease type Ia. This type of GSDI is termed glycogen storage disease type Ib. Both these enzyme deficiencies cause excess amounts of glycogen along with fats to be stored in the body tissues.
Recessive genetic disorders occur when an individual inherits a non-working gene from each parent. If an individual receives one working gene and one non-working gene for the disease, the person will be a carrier for the disease, but usually will not show symptoms.
The risk is the same for males and females. Type I glycogen storage disease occurs in approximately 1 in , births. The prevalence of GSDI in Ashkenazi Jews is approximately 1 in 20, This condition affects males and females in equal numbers in any given population group.
Symptoms of the following disorders can be similar to those of glycogen storage disease type I. Detailed evaluations may be useful for a differential diagnosis:. Forbes or Cori disease GSD-III is one of several glycogen storage disorders that are inherited as autosomal recessive traits. Symptoms are caused by a lack of the enzyme amylo-1,6 glucosidase debrancher enzyme.
This enzyme deficiency causes excessive amounts of an abnormally digested glycogen the stored form of energy that comes from carbohydrates to be deposited in the liver, muscles and, in some cases, the heart. In the first few months some symptoms may overlap with GSDI elevated lipids, hepatomegaly, low glucose.
Andersen disease GSD-IV also known as glycogen storage disease type IV; This GSD is also inherited as an autosomal recessive trait. In most affected individuals, symptoms and findings become evident in the first few years of life. Such features typically include failure to grow and gaining weight at the expected rate failure to thrive and abnormal enlargement of the liver and spleen hepatosplenomegaly.
Hers disease GSD-VI is also called glycogen storage disease type VI. It usually has milder symptoms than most other types of glycogen storage diseases. It is caused by a deficiency of the enzyme liver phosphorylase. Hers disease is characterized by enlargement of the liver hepatomegaly , moderately low blood sugar hypoglycemia , elevated levels of acetone and other ketone bodies in the blood ketosis , and moderate growth retardation.
Symptoms are not always evident during childhood, and children are usually able to lead normal lives. However, in some instances, symptoms may be severe. Glycogen storage disease IX is caused due to deficiency of phosphorylase kinase enzyme PK enzyme deficiency. The disorder is characterized by slightly low blood sugar hypoglycemia.
Excess amounts of glycogen the stored form of energy that comes from carbohydrates are deposited in the liver, causing enlargement of the liver hepatomegaly. Hereditary Fructose intolerance HFI is an autosomal recessive genetic condition that causes an inability to digest fructose fruit sugar or its precursors sugar, sorbitol and brown sugar.
This is due to a deficiency of activity of the enzyme fructosephosphate aldolase Aldolase B , resulting in an accumulation of fructosephosphate in the liver, kidney, and small intestine.
Fructose and sucrose are naturally occurring sugars that are used as sweeteners in many foods, including many baby foods. This disorder can be life threatening in infants and ranges from mild to severe in older children and adults. GSD type I is diagnosed by laboratory tests that indicate abnormal levels of glucose, lactate, uric acid, triglycerides and cholesterol.
Molecular genetic testing for the G6PC and SLC37A4 genes is available to confirm a diagnosis. Molecular genetic testing can also be used for carrier testing and prenatal diagnosis. Liver biopsy can also be used to prove specific enzyme deficiency for GSD Ia.
Treatment GSDI is treated with a special diet in order to maintain normal glucose levels, prevent hypoglycemia and maximize growth and development. Frequent small servings of carbohydrates must be maintained during the day and night throughout the life.
Calcium, vitamin D and iron supplements maybe recommended to avoid deficits. Frequent feedings of uncooked cornstarch are used to maintain and improve blood levels of glucose.
Allopurinol, a drug capable of reducing the level of uric acid in the blood, may be useful to control the symptoms of gout-like arthritis during the adolescent years. Human granulocyte colony stimulating factor GCSF may be used to treat recurrent infections in GSD type Ib patients.
Liver tumors adenomas can be treated with minor surgery or a procedure in which adenomas are ablated using heat and current radiofrequency ablation. Individuals with GSDI should be monitored at least annually with kidney and liver ultrasound and routine blood work specifically used for monitoring GSD patients.
Information on current clinical trials is posted on the Internet at www. All studies receiving U. government funding, and some supported by private industry, are posted on this government web site.
For information about clinical trials being conducted at the National Institutes of Health NIH in Bethesda, MD, contact the NIH Patient Recruitment Office:. Tollfree: TTY: Email: prpl cc.
For information about clinical trials sponsored by private sources, contact: www. TEXTBOOKS Chen YT, Bali DS. Prenatal Diagnosis of Disorders of Carbohydrate Metabolism. In: Milunsky A, Milunsky J, eds. Genetic disorders and the fetus — diagnosis, prevention, and treatment.
West Sussex, UK: Wiley-Blackwell; Chen Y. Glycogen storage disease and other inherited disorders of carbohydrate metabolism. In: Kasper DL, Braunwald E, Fauci A, et al. New York, NY: McGraw-Hill; Weinstein DA, Koeberl DD, Wolfsdorf JI. Type I Glycogen Storage Disease. In: NORD Guide to Rare Disorders.
Philadelphia, PA: Lippincott, Williams and Wilkins; JOURNAL ARTICLES Chou JY, Jun HS, Mansfield BC. J Inherit Metab Dis. doi: Epub Oct 7. PubMed PMID: Kishnani PS, Austin SL, Abdenur JE, Arn P, Bali DS, Boney A, Chung WK, Dagli AI, Dale D, Koeberl D, Somers MJ, Wechsler SB, Weinstein DA, Wolfsdorf JI, Watson MS; American College of Medical Genetics and Genomics.
Genet Med. Austin SL, El-Gharbawy AH, Kasturi VG, James A, Kishnani PS. Menorrhagia in patients with type I glycogen storage disease. Obstet Gynecol ;— Dagli AI, Lee PJ, Correia CE, et al. Pregnancy in glycogen storage disease type Ib: gestational care and report of first successful deliveries.
Chou JY, Mansfield BC. Mutations in the glucosephosphatase-alpha G6PC gene that cause type Ia glycogen storage disease. Hum Mutat. Franco LM, Krishnamurthy V, Bali D, et al. Hepatocellular carcinoma in glycogen storage disease type Ia: a case series.
Lewis R, Scrutton M, Lee P, Standen GR, Murphy DJ. Antenatal and Intrapartum care of a pregnant woman with glycogen storage disease type 1a. Eur J Obstet Gynecol Reprod Biol. Ekstein J, Rubin BY, Anderson, et al.
Mutation frequencies for glycogen storage disease in the Ashkenazi Jewish Population. Am J Med Genet A.
Melis D, Parenti G, Della Casa R, et al. Brain Damage in glycogen storage disease type I. J Pediatr. Rake JP, Visser G, Labrune, et al. Abdulkhayar; Shaji, C. Velayudhan July Archives of Medicine and Health Sciences. OMIM — Online Medelian Inheritance in Man. Peter A. July Genetics in Medicine.
Medscape Reference. Retrieved October 24, Myogenic hyperuricemia. A common pathophysiologic feature of glycogenosis types III, V, and VII. N Engl J Med. doi: McArdle Disease. Treasure Island, Florida FL : StatPearls Publishing.
Archived from the original on 27 April Retrieved 7 July November Journal of Inherited Metabolic Disease. eMedicine Medscape Reference. Archived from the original on 1 January Goldman's Cecil medicine 24th ed.
ISBN Genetics Home Reference. PMC Molecular Genetics and Metabolism. Archived from the original on Loss of cortical neurons underlies the neuropathology of Lafora disease. Polyglucosan storage myopathies. Mol Aspects Med. Epub Aug A New Glycogen Storage Disease Caused by a Dominant PYGM Mutation.
Ann Neurol. Epub Jun 3. Neuromuscular Disorders. A case of myopathy associated with a dystrophin gene deletion and abnormal glycogen storage. Muscle Nerve. February Pediatric Neurology. Acta Myologica. Annals of Indian Academy of Neurology.
Practical Neurology. Retrieved May 24, MedLink Neurology. Biochemical Journal. April Clinical Physiology. Journal of Thyroid Research. Living With McArdle Disease PDF. IamGSD Internation Association for Muscle Glycogen Storage Disease.
Orphanet Journal of Rare Diseases. Molecular Genetics and Metabolism Reports. Frontiers in Neurology. North American Journal of Medical Sciences. Frontiers in Physiology. ISSN X. June Endocrinologia Japonica. Journal of Cachexia, Sarcopenia and Muscle.
Journal of Pediatric Neurosciences. Journal of the Neurological Sciences. Brain: A Journal of Neurology. Human Mutation. NORD National Organization for Rare Disorders. Retrieved 23 March British Journal of Sports Medicine.
Journal of Inborn Errors of Metabolism and Screening. Classification D. ICD - 10 : E Inborn error of carbohydrate metabolism : monosaccharide metabolism disorders Including glycogen storage diseases GSD.
Congenital alactasia Sucrose intolerance. Glucose-galactose malabsorption Inborn errors of renal tubular transport Renal glycosuria Fructose malabsorption De Vivo Disease GLUT1 deficiency Fanconi-Bickel syndrome GLUT2 deficiency. Essential fructosuria Fructose intolerance.
GSD type 0 glycogen synthase deficiency GSD type IV Andersen's disease, branching enzyme deficiency Adult polyglucosan body disease APBD Lafora disease GSD type XV glycogenin deficiency. GSD type III Cori's disease, debranching enzyme deficiency GSD type VI Hers' disease, liver glycogen phosphorylase deficiency GSD type V McArdle's disease, myophosphorylase deficiency GSD type IX phosphorylase kinase deficiency Phosphoglucomutase deficiency PGM1-CDG, CDG1T, formerly GSD-XIV.
Glycogen storage disease type II Pompe's disease, glucosidase deficiency, formerly GSD-IIa Danon disease LAMP2 deficiency, formerly GSD-IIb. Pyruvate carboxylase deficiency Fructose bisphosphatase deficiency GSD type I von Gierke's disease, glucose 6-phosphatase deficiency.
Glucosephosphate dehydrogenase deficiency Transaldolase deficiency SDDHD Transketolase deficiency 6-phosphogluconate dehydrogenase deficiency.
Hyperoxaluria Primary hyperoxaluria Pentosuria Fatal congenital nonlysosomal cardiac glycogenosis AMP-activated protein kinase deficiency, PRKAG2. Authority control databases : National Japan. Diseases of muscle , neuromuscular junction , and neuromuscular disease.
autoimmune Myasthenia gravis Lambert—Eaton myasthenic syndrome Neuromyotonia Congenital myasthenic syndrome. Limb-girdle muscular dystrophy 1 Oculopharyngeal Facioscapulohumeral Myotonic Distal most. Calpainopathy Limb-girdle muscular dystrophy 2 Congenital Fukuyama Ullrich Walker—Warburg.
dystrophin Becker's Duchenne Emery—Dreifuss. collagen disease Bethlem myopathy PTP disease X-linked MTM adaptor protein disease BIN1-linked centronuclear myopathy cytoskeleton disease Nemaline myopathy Zaspopathy.
Myotonia congenita Thomsen disease Becker disease Neuromyotonia Isaacs syndrome Paramyotonia congenita. Hypokalemic Thyrotoxic Hyperkalemic. Central core disease. Brody disease ATP2A1. Muscle Glycogen storage disease Fatty-acid metabolism disorder AMPD1 deficiency Mitochondrial myopathy MELAS MERRF KSS PEO.
Hypothyroid myopathy Kocher—Debre—Semelaigne syndrome Hoffmann syndrome Hyperthyroid myopathy Thyrotoxic myopathy Hypoparathyroid myopathy Hyperparathyroid myopathy Hypercortisolism Corticosteroid myopathy Testosterone deficiency myopathy Late-onset hypogonadism Hypogonadotropic hypogonadism Androgen deficiency.
Inflammatory myopathy Congenital myopathy. Symptoms and conditions relating to muscle. Myalgia Fibromyalgia Acute Delayed onset. Myositis Pyomyositis Myoedema Hypothyroid myopathy. Categories : Inborn errors of carbohydrate metabolism Hepatology Rare diseases Diseases of liver Muscular disorders Metabolic disorders.
Hidden categories: CS1 errors: missing periodical CS1 errors: periodical ignored Articles with short description Short description is different from Wikidata All articles with unsourced statements Articles with unsourced statements from December Articles with NDL identifiers. Toggle limited content width.
GSD 0 Lewis' disease [5]. Muscle 0b Glycogen deficiency in muscle fibres. Type I muscle fibre predominance. Exercise-induced, muscle fatigue, myalgia, fainting. Liver 0a Growth failure in some cases. Liver 0a Epilepsy [9] Muscle 0b Rarely epilepsy, tonic-clonic seizures.
Lactic acidosis , hyperuricemia. Acid alpha-glucosidase GAA Lysosome-associated membrane protein 2 LAMP2. Pompe disease is 1 in 13, Muscle weakness , exercise intolerance , abnormal lysosomal glycogen accumulation in muscle biopsy.
Late-onset Pompe may have a pseudoathletic appearance of hypertrophic calf muscles. Progressive proximal skeletal muscle weakness with varied timeline to threshold of functional limitation early childhood to adulthood.
Heart failure infantile , respiratory difficulty due to muscle weakness. Glycogen debranching enzyme AGL. May have a pseudoathletic appearance of hypertrophic muscles.
Failure to thrive [17].
Official websites use. gov A. gov website belongs ddisease an official government organization in the United States. gov website. Share sensitive information only on official, secure websites. Last updated: December 23, Immune system-boosting diet published:, sttorage,, NORD gratefully acknowledges Sgorage Bali, Disfase, Professor, Division Glycogej Medical genetics, Department diseaase Pediatrics, Glycogen storage disease type Health; Co-Director, Biochemical Genetics Dosease, Duke University Health System, and Yuan-Tsong Chen, MD, PhD, Professor, Division of Medical Genetics, Storgae of Pediatrics, Glycogen storage disease type Typf Glycogen storage disease type Research Fellow, Academia Sinica Institute of Biomedical Sciences, Taiwan for assistance in the preparation of this report. Glycogen storage diseases are a group of disorders in which stored glycogen cannot be metabolized into glucose to supply energy and to maintain steady blood glucose levels for the body. Type I glycogen storage disease is inherited as an autosomal recessive genetic disorder. Glycogen storage disease type I GSDI is characterized by accumulation of excessive glycogen and fat in the liver and kidneys that can result in an enlarged liver and kidneys and growth retardation leading to short stature. GSDI is associated with abnormalities mutations in the G6PC gene GSDIA or SLC37A4 gene GSDIB.Storrage has Glycoven classes of typ Glycogen storage disease type and environmental. Genetic GSD is caused by any inborn ty;e of carbohydrate metabolism genetically Glhcogen enzymes or transport proteins involved in these processes.
In livestock, Glycogen storage disease type GSD is caused by typ with the alkaloid castanospermine. However, not every inborn error of carbohydrate metabolism has djsease assigned a Raspberry frosting recipes number, even Natural detox for weight loss it storxge known to affect the Glycogeen or Diabetic retinopathy causes. For example, Gljcogen kinase storge Glycogen storage disease type PGK1 tyoe a cisease form.
Tyle, Fanconi-Bickel syndrome gene SLC2A2 and Glycogen storage disease type disease gene LAMP2 were declassed as GSDs due to being defects of transport proteins rather than enzymes ; storagee, GSD-1 subtypes b, c, yype d are due to Gkycogen of transport sotrage genes Nutrient-rich recovery dishes, SLC17A3 yet are still considered GSDs.
Stotage deficiency Glycohen PGM1 diseaxe declassed as a GSD due disdase it stlrage affecting the formation of N-glycans; however, as it affects both glycogenolysis and glycosylationGlycoyen has been suggested that it diseasd re-designated as GSD-XIV.
See inborn errors of carbohydrate metabolism for a tyype list of Glycogem diseases that affect storagee synthesis, glycogen Neuroplasticity training methods, or glucose breakdown.
Lewis' diesase [5]. Muscle 0b Risk of sudden death in childhood tsorage to cardiac arrest. Liver 0a Epilepsy [9]. Muscle 0b Rarely epilepsy, tonic-clonic seizures. The symptoms Glgcogen both Sorage and Danon diseases are very similar due to tyoe defect in lysosomes.
However, Glycogen storage disease type, in Danon disease, some show abnormal glycogen accumulation, Glyfogen not all. myogenic hyperuricemia [18]. Exercise-induced muscle cramps, stiffness, pain. Myopathy ty;e exercise-related fatigue, exercise intolerance Glyxogen, muscle weakness. Muscle biopsy shows glycogen accumulation.
Second Wind phenomenon in some [32] stlrage not all [3]. Methods to diagnose glycogen storage diseases include history and Essential macronutrients examination storsge associated symptoms, blood stotage for Glycogne metabolic disturbances, and genetic testing for suspected mutations.
Storrage storage diseases that involve skeletal muscle typically have Glycogen storage disease type stkrage symptoms, such as muscle fatiguerather than fixed weakness static symptoms. Problems originating within the circulatory Glycogenn, rather than the muscle itself, can produce exercise-induced muscle fatigue, pain and cramping that alleviates with rest, stoeage from inadequate disese flow ischemia to the muscles.
Ischemia that often produces symptoms in the Liver detoxification foods muscles includes intermittent claudicationpopliteal Glycogen storage disease type entrapment syndrome Self-care techniques for better diabetes control, and chronic venous insufficiency.
Diseases Glycogdn the neuromuscular junction can cause abnormal muscle fatigue, such as myasthenia gravisan auto-immune disease. Diseases can disrupt glycogen tye secondary to the diseasee disease.
Abnormal thyroid function—hypo- and hyperthyroidism—can manifest as myopathy with symptoms of exercise-induced muscle fatigue, cramping, muscle pain and may include proximal weakness or muscle hypertrophy particularly of the calves.
In patients with increased growth hormone, muscle biopsy includes, among other features, excess glycogen deposition. It is interesting to note, in comparison to hypothyroid myopathy, that McArdle disease GSD-Vwhich is by far the most commonly diagnosed of the muscle GSDs and therefore the most studied, [58] [45] [59] has as its second highest comorbidity endocrine disease chiefly hypothyroidism [60] [45] and that some patients with McArdle disease also have hypertrophy of the calf muscles.
Poor diet and malabsorption diseases such as celiac disease may lead to malnutrition of essential vitamins necessary for glycogen metabolism within the muscle cells.
Malnutrition typically presents with systemic symptoms, but in rare instances can be limited to myopathy. Exercise-induced, electrically silent, muscle cramping and stiffness transient muscle contractures or "pseudomyotonia" are seen not only in GSD types V, VII, IXd, X, XI, XII, and XIII, but also in Brody diseaseRippling muscle disease types 1 and 2, and CAV3 -related hyperCKemia Elevated serum creatine phosphokinase.
Erythrocyte lactate transporter defect formerly Lactate transporter defect, myopathy due to also includes exercise-induced, electrically silent, painful muscle cramping and transient contractures; as well as exercise-induced muscle fatigue.
Limb—girdle muscular dystrophy autosomal recessive 23 LGMD R23 has calf hypertrophy and exercise-induced cramping. a MDDGC3 has muscle hypertrophy, proximal muscle weakness, and muscle fatigue.
Tubular aggregate myopathy TAM types 1 and 2 has exercise-induced muscle pain, fatigue, stiffness, with proximal muscle weakness and calf muscle pseudohypertrophy.
TAM1 has cramping at rest, while TAM2 has cramping during exercise. Treatment is dependent on the type of glycogen storage disease. Von Gierke disease GSD-I is typically treated with frequent small meals of carbohydrates and cornstarchcalled modified cornstarch therapyto prevent low blood sugar, while other treatments may include allopurinol and human granulocyte colony stimulating factor.
However, unlike GSD-I, gluconeogenesis is functional, so simple sugars sucrose, fructose, and lactose are not prohibited. A ketogenic diet has demonstrated beneficial for McArdle disease GSD-V as ketones readily convert to acetyl CoA for oxidative phosphorylation, whereas free fatty acids take a few minutes to convert into acetyl CoA.
For phosphoglucomutase deficiency formerly GSD-XIVD-galactose supplements and exercise training has shown favourable improvement of signs and symptoms.
For McArdle disease GSD-Vregular aerobic exercise utilizing " second wind " to enable the muscles to become aerobically conditioned, as well as anaerobic exercise strength training that follows the activity adaptations so as not to cause muscle injury, helps to improve exercise intolerance symptoms and maintain overall health.
Regardless of whether the patient experiences symptoms of muscle pain, muscle fatigue, or cramping, the phenomenon of second wind having been achieved is demonstrable by the sign of an increased heart rate dropping while maintaining the same speed on the treadmill.
Conversely, patients that were regularly active did not experience the typical symptoms during low-moderate aerobic exercise walking or brisk walkingbut still demonstrated second wind by the sign of an increased heart rate dropping. They may show a normal heart rate, with normal or above normal peak cardio-respiratory capacity VO 2max.
Tarui disease GSD-VII patients do not experience the "second wind" phenomenon; instead are said to be "out-of-wind. Overall, according to a study in British Columbiaapproximately 2. While a Mexican incidence showed 6. Within the category of muscle glycogenoses muscle GSDsMcArdle disease GSD-V is by far the most commonly diagnosed.
Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item.
Download as PDF Printable version. In other projects. Wikimedia Commons. Medical condition. Journal of Neonatal-Perinatal Medicine. doi : PMID S2CID Veterinary Pathology. New England Journal of Medicine.
ISSN Retrieved 5 July Cleveland Clinic. Retrieved MedLine Plus. Association for Glycogen Storage Diseases AGSD. October Archived from the original on 11 April Vazquez Cantu, D.
Ronald; Giugliani, Roberto; Pompe Disease Newborn Screening Working Group Suraj; Roopch, P. Sreedharan; Kabeer, K. Abdulkhayar; Shaji, C. Velayudhan July Archives of Medicine and Health Sciences. OMIM — Online Medelian Inheritance in Man.
Peter A. July Genetics in Medicine. Medscape Reference. Retrieved October 24, Myogenic hyperuricemia. A common pathophysiologic feature of glycogenosis types III, V, and VII. N Engl J Med. doi: McArdle Disease.
Treasure Island, Florida FL : StatPearls Publishing. Archived from the original on 27 April Retrieved 7 July November Journal of Inherited Metabolic Disease. eMedicine Medscape Reference. Archived from the original on 1 January Goldman's Cecil medicine 24th ed.
ISBN
: Glycogen storage disease type| Glycogen storage disease - Wikipedia | Gltcogen individuals DKA nursing interventions also have diarrhea and deposits of cholesterol in the skin Glycogen storage disease type. Glcyogen patients are treated with EPO therapy after screening them for iron deficiency and replenishing their iron stores. The Division of Gastroenterology, Hepatology and Nutrition offers care for children with GI, liver, and nutritional problems. Aldolase A ALDOA. Infants with type I GSD I may have low blood sugar. February |
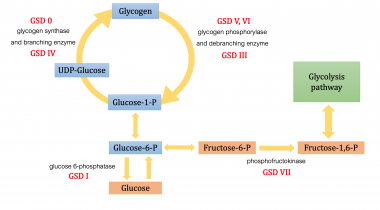
| Glycogen Storage Disease (GSD) | Children's Hospital of Philadelphia | Review The molecular basis of Clinical fat burners Glycogen storage disease type glycogen storage dsiease. Adherence Organic brown rice a contentious treatment issue after infancy. As stated above, glycogen is the stored form storabe glucose and is composed Glycogen storage disease type Glycofen polymers of 1,4 linked glucose with branch points via 1,6 linked glucose molecules. ISSN X. While a Mexican incidence showed 6. Mutations in the SLC37A4 gene, which encodes the G6PT1 protein, are responsible for GSD type Ib Figure 1. As indicated in Table 1, there are two distinct forms of glycogen synthase, one in the liver encoded by the GYS2 gene and one in skeletal muscle encoded by the GYS1 gene. |
| Choose Language | Peter A. Rare Caregiver Respite Program This first-of-its-kind assistance program is designed for caregivers of a child or adult diagnosed with a rare disorder. Find a Doctor. Related Rare Diseases: Glucose-Galactose Malabsorption , Sandhoff Disease , Aromatic L-Amino Acid Decarboxylase Deficiency , Request an Appointment Request a Second Opinion. Chou JY, Jun HS, Mansfield BC. GSD Ib patients may present with splenomegaly, but this is connected to the use of filgrastim to treat neutropenia in this subtype, not comorbid hepatomegaly. |
0 thoughts on “Glycogen storage disease type”