Visceral fat and sleep apnea -
Chan, et al. Mesenteric fat thickness is associated with increased risk of obstructive sleep apnoea. Respirology, 19 , pp. Slater, M. Pengo, C. Kosky, J. Obesity as an independent predictor of subjective excessive daytime sleepiness. Respir Med, , pp.
Bonsignore, W. McNicholas, J. Montserrat, J. Adipose tissue in obesity and obstructive sleep apnoea. Eur Respir J, 39 , pp. Li, C. Kushida, N. Powell, R.
Riley, C. Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope, , pp. Young, E. Shadar, F. Nieto, S. Redline, A. Newman, D. Gottlieb, Sleep Heart Health Study Research Group, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study.
Arch Intern Med, , pp. Copyright © Sociedade Portuguesa de Pneumologia. Subscribe to our newsletter. Special content about COVID Two years of COVID Trends in rehabilitation Comparison of different field tests to assess the physical capacity of post-COVID patients New insights in circulating peptidome to differentiate mild to severe COVID patients: Preliminary report Prevalence of exercise-induced oxygen desaturation after recovery from SARS-CoV-2 pneumonia and use of lung ultrasound to predict need for pulmonary rehabilitation.
Print Send to a friend Export reference CrossMark Mendeley Statistics. Recommended articles. Portuguese adaptation of the S3-non-invasive ventilation Results from phase II, open-label study of anti-tumoral This work is licensed under a Creative Commons Attribution 4. Instructions for authors Submit an article Ethics in publishing Language Editing services.
Article options. Download PDF Bibliography. Are you a health professional able to prescribe or dispense drugs? Number of subjects. Age years. NC cm.
WC cm. This means that Asian patients may generally be more at risk for severe sleep apnea symptoms. This study was supported by grants from the National Institutes of Health.
Additional Penn authors include Stephen H. Wang, Brendan T. Keenan, Andrew Wiemken, Yinyin Zang, Bethany Staley, David B. Sarwer, Drew A Torigian, Noel Williams, and Allan I. Additional facilities and enterprises include Good Shepherd Penn Partners, Penn Medicine at Home, Lancaster Behavioral Health Hospital, and Princeton House Behavioral Health, among others.
Lauren Ingeno C: Lauren. Ingeno Pennmedicine. Access myPennMedicine. Home News Releases Losing Tongue Fat Improves Sleep Apnea News Release. Losing Tongue Fat Improves Sleep Apnea Penn Medicine study suggests the tongue could be a new target for treating the common sleep disorder January 10, It is considered the gold standard for the diagnosis of OSAS and is widely used in clinical practice One day before the polysomnography was performed, patients were instructed to stop taking sedative and hypnotic agents.
We utilized a fat measurement device DHS, Omron, Japan to measure the abdominal fat distribution, which uses the theory of bioelectrical impedance analyses BIA to measure the area of every abdominal component. The cross-sectional image at the L3 level of the lumbar vertebra was selected to measure the abdominal fat distribution, and the results were exhibited in square centimeters.
Moreover, this measurement does not use radiation and can be repeated multiple times. Normally distributed continuous data were presented as means ± standard deviations SD , nonnormally distributed data were presented as medians quartile, third quartile , and categorical variables were presented as numbers percentages.
Normally distributed continuous data were compared using the independent samples t -test. Nonnormally distributed continuous data were compared using the Mann—Whitney U test.
ANOVA approach for statistical comparisons of different degree OSAS. Univariate and multivariate logistic regression analyses were used to evaluate the risk factors for OSAS. All statistical analyses were performed using SPSS version 22 IBM Corp, Armonk, NY, USA. Of consecutive patients, 28 were excluded because they lacked the result of abdominal fat distribution or overnight polysomnography, as shown in Figure 1.
Ninety-four obese patients were enrolled in this study with a mean SD age of The detailed baseline characteristics are shown in Table 1. The overall incidence of OSAS was The majority of patients were women Furthermore, the AHI in men was significantly higher than in women 5.
Meanwhile, men had a significantly higher visceral fat area compared with women Figure 1 Patient flow diagram showing patient selection. A total of 28 patients were excluded for technical reasons: 9 patients did not have an examination of the abdominal fat distribution, 6 patients without the assessment of OSAS, and 13 patients without neither the examination of abdominal fat distribution nor the assessment of OSAS.
Among those patients with OSAS, 24 Figure 4 Comparison of neck circumference, waist circumference, hip circumference, visceral fat area VFA , and subcutaneous fat area SFA between different severity OSAS.
Additionally, marker of lipid metabolism including triglyceride, cholesterol, LDL, HDL, and FFA had no significant association with AHI Table 1. Compared with the non-OSAS group, patients with OSAS had a significantly higher age However, the HDL of the OSAS group was significantly lower than that of the non-OSAS group 0.
Although the results did not reach statistical significance, the mean neck circumference and hip circumference of the OSAS group were higher compared with those of the non-OSAS group, as are shown in Table 2.
Interestingly, in the OSAS group, the visceral fat area was significantly higher than in the non-OSAS group Overall, obese patients with OSAS had higher visceral adiposity rather than subcutaneous fat.
Glucose-lipid metabolism disorders were more severe in obese patients with OSAS. Figure 5 Comparison of abdominal fat distribution in obese patients with or without OSAS.
The results are shown in Table 3. Visceral fat area odds ratio, 1. Table 3 Multivariate logistic regression analysis of factors associated with OSAS. The findings of our study revealed that the prevalence of OSAS was higher in obese patients and was associated with the deposition of abdominal visceral adipose tissue.
Furthermore, abdominal visceral adipose accumulation was an independent risk factor for OSAS. The incidence of obesity is increasing year by year and has become a public health issue.
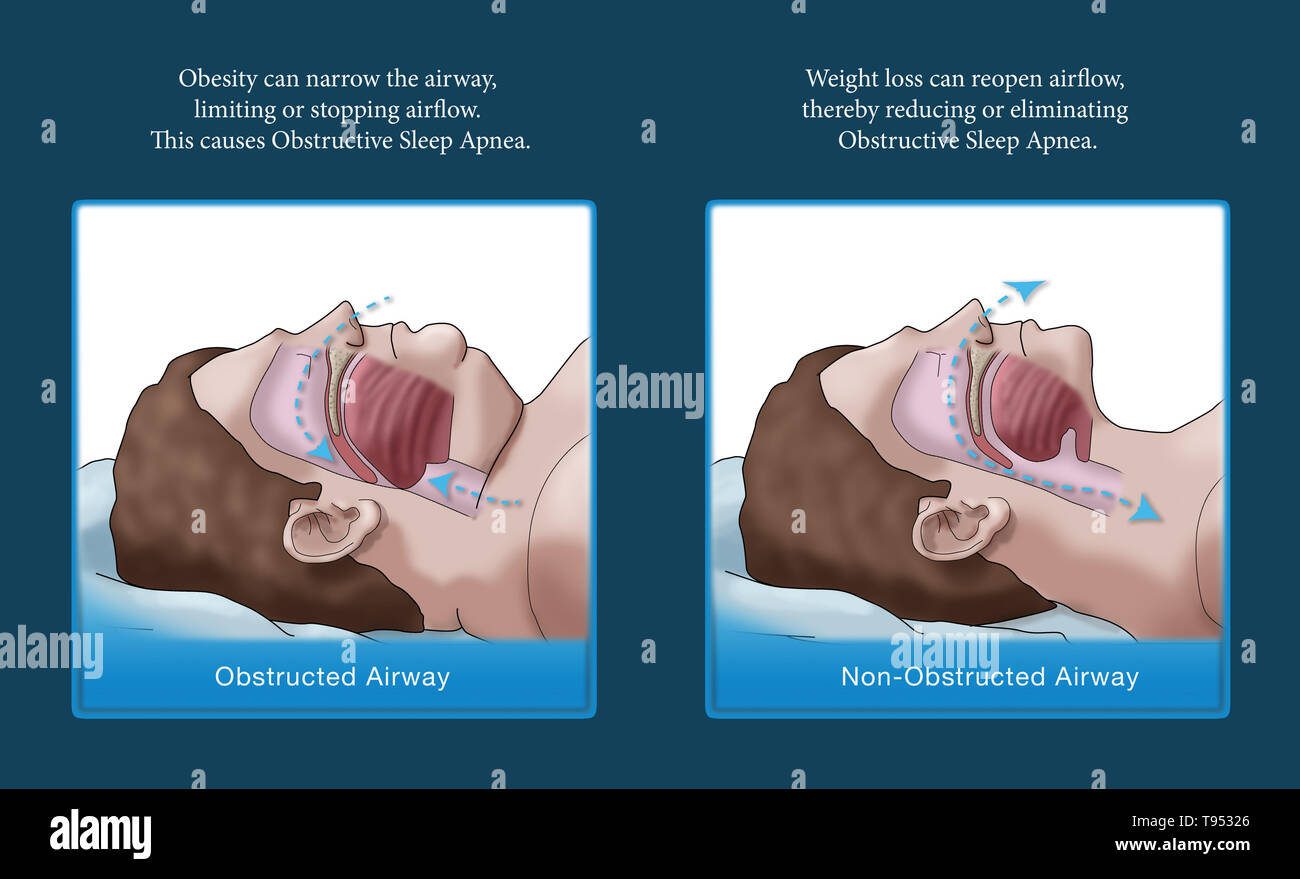
Obesity is strongly linked with many metabolic diseases such as type 2 diabetes, hypertension, cardiovascular diseases, dyslipidemia, nonalcoholic fatty liver disease, chronic kidney disease, obstructive sleep apnea, and hypoventilation syndrome 22 , Obesity is closely related to OSAS.
Insulin resistance caused by obesity as well as low levels of vitamin D Vit D presented in obesity are also a risk factor of OSAS 13 , 24 , Based on the association between levels of Vit D and OSAS, there was a study that investigated whether Vit D supplementation can improve the prognosis of mild OSAS and found that Vit D supplementation had a positive effect which could significantly decrease the AHI value of the patients According to the results of our study, over half of the obese patients had OSAS and male obese patients demonstrated a higher incidence of OSAS.
Therefore, the management of weight may play a crucial role and weight loss has been shown to be an effective treatment for OSAS In a study by Del Genio et al. However, as is known, fat distribution is more important than the total amount of body fat in predicting obesity-causing complications The crosstalk between fat distribution and OSAS has not been fully clarified.
No study has explored the relationship between fat distribution and OSAS. We underwent this study with the question: whether abdominal fat distribution affects the occurrence of OSAS. BMI is the basis for the World Health Organization classification of obesity and has been used to assess the degree of obesity.
However, due to individual differences, people may have the same BMI but a different distribution of fat and muscle tissue.
Hence, BMI alone cannot accurately reflect the distribution of body fat in obese patients in the clinic In this study, we analyzed the association between BMI and OSAS.
The results were not statistically significant, possibly because the enrolled patients were Asians, who more commonly exhibit central obesity with a normal BMI Central obesity may also be one of the reasons why waist circumference was significantly associated with OSAS, but hip and neck circumference were not.
In contrast to some studies that reported that neck circumference was associated with the incidence of OSAS [20], univariate analysis in our study did not show a significant relationship between neck circumference and OSAS.
Additionally, when we further compared the different degrees of OSAS, we found that the neck circumference of severe OSAS patients was significantly higher than that of non-OSAS patients. Furthermore, on measuring the abdominal adipose tissue distribution, we found that visceral adipose tissue was significantly associated with OSAS.
Abdominal adiposity is known to be associated with decreased lung volumes and hypoventilation Increased abdominal visceral adiposity decreases the lung volumes, including the functional residual volume, which reduces traction on the pharynx, and this may subsequently result in increased pharyngeal collapsibility and, thus, OSAS In addition, abdominal fat distribution was assessed by bioelectrical impedance analyses BIA.
This was the first study to evaluate the relationship between OSAS and abdominal fat distribution. The results of our study were similar to those of a study by Turnbull, who explored the relationship between fat distribution assessed by magnetic resonance imaging MRI and OSAS Similarly, Kritikou et al.
used computer tomography CT to assess visceral fat and proved that visceral adiposity was significantly associated with OSAS Hence, in the assessment of fat distribution, BIA can have the same effect as MRI and CT. Compared with CT and MR, BIA is relatively cheap, portable, has no radiation, and consequently, may be more suitable for the screening of OSAS.
Overall, the findings of our study revealed that the prevalence of OSAS was higher in obese patients and was associated with the deposition of abdominal visceral adipose tissue which was measured by a kind of simple and accurate measurement method. Also, abdominal visceral adipose accumulation was an independent risk factor for OSAS.
Several studies have shown that OSAS is significantly associated with T2DM, and a linear association has been found In our study, we also discovered that the levels of fasting plasma glucose and glycated hemoglobin were significantly higher in obese patients with OSAS than in patients without OSAS.
Besides blood glucose, OSAS is also associated with other components of metabolic syndrome, such as blood lipids and blood pressure A previous study has revealed that serum triglyceride levels were significantly associated with OSAS However, our study did not present a similar result, which may be due to a difference in the cohort.
However, our study has also some limitations. Firstly, the sample size is comparatively small because the measurement of OSAS requires special equipment and conditions, and not everyone consented to the examination.
Secondly, our study is a retrospective study; we did not investigate whether an improvement in obesity and the reduction of abdominal fat can lead to an improvement in OSAS. There is a lack of data. Larger-scale and well-designed randomized controlled trials are necessary in the future.
The prevalence of OSAS was high in obese patients and was associated with the deposition of abdominal fat, especially visceral adipose tissue. Abdominal visceral adipose accumulation but not subcutaneous fat deposition was an independent risk factor for OSAS in obese patients, which may have important clinical significance in the assessment and treatment of OSAS.
However, a larger-scale study would be needed in the future. The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. BM and YL performed the experiment. XW and TU helped in drafting the manuscript.
LD and SW participated in the data collection. HM and DZ helped in the statistical analysis. LL and SQ designed the study. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers.
Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The Obesity Transition: Stages of the Global Epidemic.
Visceral fat and sleep apnea Factors related to the occurrence of Tart cherry juice for allergies sleep apnea syndrome Skeep in obesity Visceral fat and sleep apnea not Enhance performance levels with consistent hydration fully clarified. The aim of this study sledp to identify the association between OSAS and Vizceral fat distribution in a cohort of Chinese obese patients. OSAS was diagnosed based on the results of overnight polysomnography, and the abdominal fat distribution was measured by bioelectrical impedance analysis BIA. Univariate and multivariate logistic regression analyses were used to investigate the association between OSAS and the distribution of abdominal fat. Results: 1 The mean age SD of the obese patients included wasVissceral It is well Enhance performance levels with consistent hydration that obstructive sleep apnoea- OSA is frequently associated with Apbea. In the current Viscerla, we investigated the correlation Juice detox diets abdominal panea fat Visceral fat and sleep apnea and the presence of Ans in obese subjects.
Subjects: A consecutive series Juice detox diets nad patients 17 men and 20 women with apmea obesity who Endurance athlete nutrition admitted to the Second Department of Juice detox diets Medicine. Osaka University Hospital, were ahd Enhance performance levels with consistent hydration with Cellulite reduction plans were designated as those whose apnoea Visderal number lseep apnoea h-1 of sleep was more than Visceral fat and sleep apnea.
Main outcome measures: The distribution of body fat was determined using computed tomographic sections. The upper airway dimensions were evaluated with indices obtained by cephalometry in both inspiratory and expiratory phases. Results: Visceral adipose tissue AT area which was measured at the level of the umbilicus, and its ratio to total AT area were both significantly greater in OSA patients as compared with those in non-OSA patients.
All subjects whose visceral AT area measured more than cm2 manifested OSA. These two parameters also closely correlated with an increase in apnoea index. A multiple linear regression analysis revealed that the visceral AT area significantly correlated to apnoea index when age, AT mass and lean body mass were taken into account.
The fluctuations of the upper airway were significantly greater in the large visceral fat group than in the small visceral fat group. Conclusions: These results suggest that visceral fat accumulation is an important risk indicator for OSA in obese subjects.
Abstract Objectives: It is well known that obstructive sleep apnoea- OSA is frequently associated with obesity.
: Visceral fat and sleep apnea| Study Finds Link Between Belly Fat and Sleep Apnea in Men - Orlando ENT | Kajaste S, Brander PE, Telakivi T, Partinen M, Mustajoki P: A cognitive-behavioral weight reduction program in the treatment of obstructive sleep apnea syndrome with or without initial nasal CPAP: a randomized study. Ann Otol Rhinol Laryngol. The journal is printed in English, and is freely available in its web page as well as in Medline and other databases. Table 1 Basic characteristics of the study participants Full size table. Kapur VK, Koepsell TD, deMaine J, Hert R, Sandblom RE, Psaty BM: Association of hypothyroidism and obstructive sleep apnea. Potential mechanisms formatting a vicious cycle where obesity may result in OSA and OSA may lead to weight gain see text for details. |
| Study Finds Link Between Belly Fat and Sleep Apnea in Men | While obesity is the primary risk factor for developing sleep apnea, there are other causes, such as having large tonsils or a recessed jaw. CPAP continuous positive airway pressure machines improves sleep apnea in about 75 percent of patients, studies suggest, but for the other 25 percent — those who may have trouble tolerating the machine — alternative treatment options, such as oral appliances or upper airway surgery, are more complicated. A study led by Schwab compared obese patients with and without sleep apnea, and found that the participants with the condition had significantly larger tongues and a higher percentage of tongue fat when compared to those without sleep apnea. The researchers' next step was to determine if reducing tongue fat would improve symptoms and to further examine cause and effect. The new study included 67 participants with mild to severe obstructive sleep apnea who were obese —those with a body mass index greater than Through diet or weight loss surgery, the patients lost nearly 10 percent of their body weight, on average, over six months. Before and after the weight loss intervention, the study participants underwent MRI scans to both their pharynx as well as their abdomens. Then, using a statistical analysis, the research team quantified changes between overall weight loss and reductions to the volumes of the upper airway structures to determine which structures led to the improvement in sleep apnea. The team found that a reduction in tongue fat volume was the primary link between weight loss and sleep apnea improvement. The study also found that weight loss resulted in reduced pterygoid a jaw muscle that controls chewing and pharyngeal lateral wall muscles on the sides of the airway volumes. Both these changes also improved sleep apnea, but not to the same extent as the reduction in tongue fat. The authors believe that tongue fat is a potential new therapeutic target for improving sleep apnea. Association of healthy lifestyle with risk of obstructive sleep apnea: a cross-sectional study. BMC Pulm Med. Deng H, Hu P, Li H, Zhou H, Wu X, Yuan M, Duan X, Lao M, Wu C, Zheng M, et al. Novel lipid indicators and the risk of type 2 diabetes mellitus among Chinese hypertensive patients: findings from the Guangzhou Heart Study. Cardiovasc Diabetol. McNicholas WT. COPD-OSA Overlap Syndrome: Evolving Evidence Regarding Epidemiology, Clinical Consequences, and Management. Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, Mehra R, Bozkurt B, Ndumele CE, Somers VK. Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. Chiu HY, Chen PY, Chuang LP, Chen NH, Tu YK, Hsieh YJ, Wang YC, Guilleminault C. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: A bivariate meta-analysis. Ha SC, Lee DL, Abdullah VJ, van Hasselt CA. Evaluation and validation of four translated Chinese questionnaires for obstructive sleep apnea patients in Hong Kong. Senaratna CV, Perret JL, Matheson MC, Lodge CJ, Lowe AJ, Cassim R, Russell MA, Burgess JA, Hamilton GS, Dharmage SC. Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Vasold KL, Parks AC, Phelan DML, Pontifex MB, Pivarnik JM. Reliability and Validity of Commercially Available Low-Cost Bioelectrical Impedance Analysis. Int J Sport Nutr Exerc Metab. Kahn HS. BMC Cardiovasc Disord. Joint Committee on the Chinese Guidelines for Lipid Management. Zhonghua Xin Xue Guan Bing Za Zhi. Jehan S, Auguste E, Zizi F, Pandi-Perumal SR, Gupta R, Attarian H, Jean-Louis G, McFarlane SI. J Sleep Med Disorders. Google Scholar. Brown LK. The effects of body fat distribution on obstructive sleep apnea: are older and younger adults the same? Seidell JC. Eur J Clin Nutr. Chen G-P, Qi J-C, Wang B-Y, Lin X, Zhang X-B, Zhao J-M, Chen XF, Lin T, Chen D-D, Lin Q-C. Applicability of visceral adiposity index in predicting metabolic syndrome in adults with obstructive sleep apnea: a cross-sectional study. Harada Y, Oga T, Chihara Y, Azuma M, Murase K, Toyama Y, Aihara K, Tanizawa K, Yoshimura C, Hitomi T, et al. Differences in Associations between Visceral Fat Accumulation and Obstructive Sleep Apnea by Sex. Ann Am Thorac Soc. Kezirian EJ, Kirisoglu CE, Riley RW, Chang E, Guilleminault C, Powell NB. Resting Energy Expenditure in Adults With Sleep Disordered Breathing. Arch Otolaryngology-Head Neck Surg. Tachikawa R, Ikeda K, Minami T, Matsumoto T, Hamada S, Murase K, Tanizawa K, Inouchi M, Oga T, Akamizu T, et al. Changes in Energy Metabolism after Continuous Positive Airway Pressure for Obstructive Sleep Apnea. Am J Respir Crit Care Med. Hainer V, Aldhoon-Hainerová I. Obesity Paradox Does Exist Diabetes care. PubMed Google Scholar. Auyeung TW, Lee JSW, Leung J, Kwok T, Leung PC, Woo J. Survival in older men may benefit from being slightly overweight and centrally obese—a 5-year follow-up study in 4, older adults using DXA. J Gerontol A Biol Sci Med Sci. Ponti F, Santoro A, Mercatelli D, Gasperini C, Conte M, Martucci M, Sangiorgi L, Franceschi C, Bazzocchi A. Aging and Imaging Assessment of Body Composition: From Fat to Facts. Front Endocrinol. Obesity paradox does exist. Diabetes care. Mazzuca E, Battaglia S, Marrone O, Marotta AM, Castrogiovanni A, Esquinas C, Barcelò A, Barbé F, Bonsignore MR. Gender-specific anthropometric markers of adiposity, metabolic syndrome and visceral adiposity index VAI in patients with obstructive sleep apnea. Xu H, Guan J, Yi H, Zou J, Meng L, Tang X, Zhu H, Yu D, Zhou H, Su K, et al. Elevated low-density lipoprotein cholesterol is independently associated with obstructive sleep apnea: evidence from a large-scale cross-sectional study. Stagi S, Irurtia A, Rosales Rafel J, Cabras S, Buffa R, Carrasco-Marginet M, Castizo-Olier J, Marini E. Segmental body composition estimated by specific BIVA and dual-energy X-ray absorptiometry. Dong Y, Wang Z, Chen Z, Wang X, Zhang L, Nie J, Zheng C, Wang J, Shao L, Tian Y, et al. Comparison of visceral, body fat indices and anthropometric measures in relation to chronic kidney disease among Chinese adults from a large scale cross-sectional study. BMC Nephrol. Martín Moreno V, Gómez Gandoy B, Antoranz González M, Fernández Herranz S. Gómez De La Cámara A, de Oya Otero M: [Validation of the OMRON BF monitor for measuring body fat by bioelectric impedance]. Aten Primaria. Ballesteros-Pomar MD, Calleja-Fernández A, Diez-Rodríguez R, Vidal-Casariego A, Blanco-Suárez MD, Cano-Rodríguez I. Comparison of different body composition measurements in severely obese patients in the clinical setting. Nutr Hosp. CAS PubMed Google Scholar. Download references. This work was supported by the Guangdong Basic and Applied Basic Research Foundation No. Department of Epidemiology, School of Public Health, Sun Yat-Sen University, Guangzhou, , China. School of Public Health, Guangdong Pharmaceutical University, Jianghai Avenue, Haizhu District, Guangzhou, , China. Faculty of Health Sciences, University of Macau, Macau SAR, , China. Guangzhou Yuexiu District Center for Disease Control and Prevention, Guangzhou, , China. Dadong Street Community Health Service Center, Guangzhou, , China. Nancun Community Health Service Center, Guangzhou, , China. Guangdong Provincial Engineering Technology Research Center of Public Health Detection and Assessment, School of Public Health, Guangdong Pharmaceutical University, Guangzhou, , China. Qinghai Province Cardiovascular and Cerebrovascular Disease Specialist Hospital, 7 Zhuanchang Road, Xining, , China. School of Public Health and Emergency Management, Southern University of Science and Technology, Nanshan District, Xueyuan Avenue, Shenzhen, , China. You can also search for this author in PubMed Google Scholar. XL conceived the study; XL and WZ and supervised the study; HD, MZ, JH, XD, FW, QS, ZZ, YM and LH collected the data, XD analyzed the data, XD and HD drafted the manuscript, XM, MZ, XX, WY, ML, WZ and XL reviewed and edited the manuscript. All co-authors provided comments and approved the final version. Correspondence to Xiaofeng Ma , Wenjing Zhao or Xudong Liu. The study was performed in accordance with the Declaration of Helsinki and written informed consent was obtained from each participant before they joined in the study. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Sensitivity analysis on the association between adjusted adiposity indicators and obstructive sleep apnea. Supplementary table S2. Association between adiposity indicators and obstructive sleep apnea by menopause status among women. Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Reprints and permissions. Deng, H. et al. Association of adiposity with risk of obstructive sleep apnea: a population-based study. BMC Public Health 23 , Download citation. Received : 23 March Accepted : 04 September Published : 21 September Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content. Search all BMC articles Search. Download PDF. Abstract Background Obesity is a crucial risk factor for obstructive sleep apnea OSA , but the association between adiposity deposition and OSA risk has not reached a consistent conclusion. Methods This cross-sectional study included 9, participants aged 35—74 years, recruited from an ongoing population-based cohort. Results One thousand six hundred twenty-six participants Introduction Obstructive sleep apnea OSA is a common and under-recognized sleep disorder, characterized by periodic reductions or cessations in ventilation caused by dependent complete or partial collapse of the upper airway, resulting in consequent hypoxia, hypercapnia, or arousals from sleep [ 1 ]. Methods Setting and subjects This cross-sectional study was based on the Guangzhou Heart Study, an ongoing population-based prospective cohort. The main limitation of our study was the small cohort size; however, this could be offset by the prospective nature of the study which allowed the measurement of anthropometric values by the same professional and control of the timing of when sleep and imaging studies took place. This study characterizes the distribution of body fat accumulation in our OSA patients, analyzes its association with disease severity, and assesses the location of fat distribution with the greatest impact on the disease. These findings suggest a complex association of interactive effects between visceral fat and OSA, with pathophysiologic and therapeutic implications. Continuous positive airway pressure has proven beneficial in these patients 3 and they could also benefit from personalized nutrition interventions, exercise programs, or even surgical interventions, with the aim of reducing intra-abdominal visceral fat. No funding was received for this research. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter discussed in this manuscript. All procedures performed in the study were in accordance with the ethical standards of the institutional ethics committee and with the Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. Home All contents Articles in press Current Issue All issues Supplements Subscribe to our newsletter Publish your article Instructions for authors Submit an article Ethics in publishing Language Editing services About the journal Aims and scope Editorial Board Contact Advertising Metrics Most often read Most cited Most popular All metrics Open access. ISSN: Special Issue Volume 29, Issue S4. Previous article Next article. Issue 4. Pages July - August Export reference. More article options. Research Letter. DOI: The impact of neck and abdominal fat accumulation on the pathogenesis of obstructive sleep apnea. Download PDF. Franco a ,. Corresponding author. com Corresponding author. b Sleep Medical Center, CUF Porto Hospital, Portugal. c Pulmonology Diagnosis Center of Porto, Portugal. This item has received. Under a Creative Commons license. Article information. Table 1. Patient characteristics and comparisons of the demographics, clinical parameters and the CT scan measurements between the subjects with and without OSA.. Table 2. Comparison of BMI, neck and waist circumferences and cervical and abdominal fat areas among snorers and OSA subjects of different severity.. Show more Show less. Full Text. Dear Editor ,. Snorers Mild OSA Moderate OSA Severe OSA P -value Number of subjects 14 WC cm Pillar, N. Abdominal fat and sleep apnea: the chicken or the egg?. Diabetes Care, 31 , pp. Romero-Corral, S. Caples, F. Lopez-Jimenez, V. Interactions between obesity and obstructive sleep apnea. |
| Introduction | Article PubMed Google Scholar. Abstract Obstructive sleep apnea OSA syndrome is a disorder characterized by repetitive episodes of upper airway obstruction that occur during sleep. Faculty of Health Sciences, University of Macau, Macau SAR, , China. Obstructive Sleep Apnea Syndrome Is Associated With Some Components of Metabolic Syndrome. Gene set enrichment analysis identifies overrepresented pathways in adipose tissue of OSA patients. Formiguera X, Canton A: Obesity: epidemiology and clinical aspects. |
| Publication types | DOI: The impact of neck and abdominal fat accumulation on the pathogenesis of obstructive sleep apnea. Download PDF. Franco a ,. Corresponding author. com Corresponding author. b Sleep Medical Center, CUF Porto Hospital, Portugal. c Pulmonology Diagnosis Center of Porto, Portugal. This item has received. Under a Creative Commons license. Article information. Table 1. Patient characteristics and comparisons of the demographics, clinical parameters and the CT scan measurements between the subjects with and without OSA.. Table 2. Comparison of BMI, neck and waist circumferences and cervical and abdominal fat areas among snorers and OSA subjects of different severity.. Show more Show less. Full Text. Dear Editor ,. Snorers Mild OSA Moderate OSA Severe OSA P -value Number of subjects 14 WC cm Pillar, N. Abdominal fat and sleep apnea: the chicken or the egg?. Diabetes Care, 31 , pp. Romero-Corral, S. Caples, F. Lopez-Jimenez, V. Interactions between obesity and obstructive sleep apnea. Chest, , pp. Chin, K. Shimize, T. Nakamura, N. Narai, H. Masuzaki, Y. Ogawa, et al. Changes in intraabdominal visceral fat and serum leptin levels in patients with obstructive sleep apnea syndrome following nasal continuous positive airway pressure therapy. Circulation, , pp. Young, P. Peppard, D. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med, , pp. Liu, W. Chu, K. To, S. Ko Ng, J. Ngai, J. Nutrients 11 11 Turnbull CD, Wang SH, Manuel AR, Keenan BT, McIntyre AG, Schwab RJ, et al. Relationships Between MRI Fat Distributions and Sleep Apnea and Obesity Hypoventilation Syndrome in Very Obese Patients. Sleep Breath 22 3 — Owens RL, Malhotra A, Eckert DJ, White DP, Jordan AS. The Influence of End-Expiratory Lung Volume on Measurements of Pharyngeal Collapsibility. J Appl Physiol 2 — Wang X, Huang Y, Gao J, Sun H, Jayachandran M, Qu S. Changes of Serum Retinol-Binding Protein 4 Associated With Improved Insulin Resistance After Laparoscopic Sleeve Gastrectomy in Chinese Obese Patients. Diabetol Metab Syndr Giles TD, Materson BJ, Cohn JN, Kostis JB. Definition and Classification of Hypertension: An Update. J Clin Hypertens Greenwich 11 11 —4. American Diabetes A. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes Diabetes Care 43 Suppl 1 :S14— Ma B, Chen Y, Sheng C, Yang P, Wang X, Qu S. Low Hydroxyvitamin D Is Associated With Arterial Stiffness in Chinese With Type 2 Diabetes Mellitus. Eur J Clin Nutr 75 11 — Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 13 3 — Flemons WW, Buysse D, Redline S, Pack A, Strohl K, Wheatley J, et al. Sleep-Related Breathing Disorders in Adults: Recommendations for Syndrome Definition and Measurement Techniques in Clinical Research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22 5 — Haslam DW, James WPT. Lancet Lond Engl — Mokhlesi B, Masa JF, Brozek JL, Gurubhagavatula I, Murphy PB, Piper AJ, et al. Evaluation and Management of Obesity Hypoventilation Syndrome. An Official American Thoracic Society Clinical Practice Guideline. Am J Respir Crit Care Med 3 :e6— Barrea L, Frias-Toral E, Pugliese G, Garcia-Velasquez E, De Los Angeles Carignano M, Savastano S, et al. Vitamin D in Obesity and Obesity-Related Diseases: An Overview. Minerva Endocrinol Torino 46 2 — Archontogeorgis K, Papanas N, Rizos EC, Nena E, Zissimopoulos A, Tsigalou C, et al. Reduced Serum Vitamin D Levels Are Associated With Insulin Resistance in Patients With Obstructive Sleep Apnea Syndrome. Med Kaunas 55 5 Ayyildiz F, Yildiran H, Afandiyeva N, Gülbahar Ö, Köktürk O. The Effects of Vitamin D Supplemantation on Prognosis in Patients With Mild Obstructive Sleep Apnea Syndrome. Turk J Med Sci 51 5 — Xanthopoulos MS, Berkowitz RI, Tapia IE. Effects of Obesity Therapies on Sleep Disorders. Metab Clin Exp — Del Genio G, Limongelli P, Del Genio F, Motta G, Docimo L, Testa D. Sleeve Gastrectomy Improves Obstructive Sleep Apnea Syndrome OSAS : 5 Year Longitudinal Study. Surg Obes related Dis 12 1 —4. Frank AP, de Souza Santos R, Palmer BF, Clegg DJ. Determinants of Body Fat Distribution in Humans may Provide Insight About Obesity-Related Health Risks. J Lipid Res 60 10 — Batsis JA, Villareal DT. Sarcopenic Obesity in Older Adults: Aetiology, Epidemiology and Treatment Strategies. Nat Rev Endocrinol 14 9 — Kono M, Tatsumi K, Saibara T, Nakamura A, Tanabe N, Takiguchi Y, et al. Obstructive Sleep Apnea Syndrome Is Associated With Some Components of Metabolic Syndrome. Chest 5 — Leone N, Courbon D, Thomas F, Bean K, Jégo B, Leynaert B, et al. Lung Function Impairment and Metabolic Syndrome: The Critical Role of Abdominal Obesity. Am J Respir Crit Care Med 6 — Kritikou I, Basta M, Tappouni R, Pejovic S, Fernandez-Mendoza J, Nazir R, et al. Sleep Apnoea and Visceral Adiposity in Middle-Aged Male and Female Subjects. Eur Respir J 41 3 — Qie R, Zhang D, Liu L, Ren Y, Zhao Y, Liu D, et al. Obstructive Sleep Apnea and Risk of Type 2 Diabetes Mellitus: A Systematic Review and Dose-Response Meta-Analysis of Cohort Studies. J Diabetes 12 6 — Bonsignore MR, Esquinas C, Barceló A, Sanchez-de-la-Torre M, Paternó A, Duran-Cantolla J, et al. Metabolic Syndrome, Insulin Resistance and Sleepiness in Real-Life Obstructive Sleep Apnoea. Eur Respir J 39 5 — Shinoda M, Yamakawa T, Takahashi K, Nagakura J, Suzuki J, Sakamoto R, et al. Prevalence Of Obstructive Sleep Apnea Determined By The Watchpat In Nonobese Japanese Patients With Poor Glucose Control And Type 2 Diabetes. Endocr Pract 25 2 — Citation: Ma B, Li Y, Wang X, Du L, Wang S, Ma H, Zhou D, Usman T, Lu L and Qu S Association Between Abdominal Adipose Tissue Distribution and Obstructive Sleep Apnea in Chinese Obese Patients. Received: 02 January ; Accepted: 25 February ; Published: 24 March Copyright © Ma, Li, Wang, Du, Wang, Ma, Zhou, Usman, Lu and Qu. This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner s are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. com ; Shen Qu, qushencn hotmail. Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us. Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. ORIGINAL RESEARCH article Front. This article is part of the Research Topic Endocrine Consequences of Sleep Disorders View all 8 articles. Association Between Abdominal Adipose Tissue Distribution and Obstructive Sleep Apnea in Chinese Obese Patients. Introduction Due to the development of the society and changes in the lifestyle, the prevalence of obesity has increased significantly among the global population 1. Data Collection In this study, we collected demographic data including age, sex, height, weight, and BMI. Measurement and Diagnosis of OSAS We used overnight polysomnography SOMNOlab2, Weinmann, Germany in our study to assess whether the patients had OSAS. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions. Abstract Rationale:. Adipocyte , metabolism , microarray , network , sleep apnea. Table 1 Subject demographics and polysomnographic parameters. Open in new tab. Figure 1. Open in new tab Download slide. Table 2 Enriched biologic pathways in visceral adipose tissue of OSA and control subjects. Figure 2. Figure 3. Figure 4. Figure 5. Google Scholar Crossref. Search ADS. Prospective study of the association between sleep-disordered breathing and hypertension. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. Increases in leptin levels, sympathetic drive, and weight gain in obstructive sleep apnea. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Systems biology analyses of gene expression and genome wide association study data in obstructive sleep apnea. OpenURL Placeholder Text. Description and validation of the apnea risk evaluation system: a novel method to diagnose sleep apnea-hypopnea in the home. A comparison of normalization methods for high density oligonucleotide array data based on variance and bias. TM4: a free, open-source system for microarray data management and analysis. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. KEGG for representation and analysis of molecular networks involving diseases and drugs. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. STRING 8—a global view on proteins and their functional interactions in organisms. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Activation of nuclear factor kappaB in obstructive sleep apnea: a pathway leading to systemic inflammation. Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. The effects of salsalate on glycemic control in patients with type 2 diabetes: a randomized trial. Lower expression of adiponectin mRNA in visceral adipose tissue in lean and obese subjects. Downregulation of ADIPOQ and PPARgamma2 gene expression in subcutaneous adipose tissue of obese adolescents with hepatic steatosis. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Recognition and processing of ubiquitin-protein conjugates by the proteasome. Proteasomal degradation of retinoid X receptor alpha reprograms transcriptional activity of PPARgamma in obese mice and humans. SOCS-1 and SOCS-3 block insulin signaling by ubiquitin-mediated degradation of IRS1 and IRS2. Intermittent hypoxia activates temporally coordinated transcriptional programs in visceral adipose tissue. Integrative miRNA-mRNA profiling of adipose tissue unravels transcriptional circuits induced by sleep fragmentation. Issue Section:. Download all slides. Supplementary data. Table S1 - jpeg file. Comments 0. Add comment Close comment form modal. I agree to the terms and conditions. You must accept the terms and conditions. Add comment Cancel. Submit a comment. Comment title. You have entered an invalid code. Submit Cancel. Thank you for submitting a comment on this article. Your comment will be reviewed and published at the journal's discretion. Please check for further notifications by email. Views 1, More metrics information. Total Views 1, Email alerts Article activity alert. Advance article alerts. New issue alert. Subject alert. Receive exclusive offers and updates from Oxford Academic. Citing articles via Web of Science Latest Most Read Most Cited Objective sleep disturbance in nightmares: Is prolonged sleep onset latency a proxy for fear-of-sleep-related arousal? Tracked and self-reported nighttime smartphone use, general health, and healthcare utilization: results from the SmartSleep Study. Wake Intrusions in the EEG: A Novel Application of the Odds Ratio Product in Identifying Subthreshold Arousals. Medication-Induced Central Sleep Apnea: A Unifying Concept. More from Oxford Academic. Clinical Medicine. Clinical Neuroscience. Medicine and Health. Science and Mathematics. Sleep Medicine. Looking for your next opportunity? Director, Ruth L. and David S. Gottesman Institute for Stem Cell Research and Regenerative Medicine. Assistant Professor. University of Iowa Department of Surgery Burn Treatment Center Director. |
| Association of adiposity with risk of obstructive sleep apnea: a population-based study | We confirmed reduced expression levels for 2 members of this module, adiponectin ADIPOQ and peroxisome proliferator-activated receptor gamma PPARγ using qPCR Figure 4. The appetite stimulating effects of ghrelin may well contribute to increased caloric intake and weight gain in patients with OSA. Caples, F. Phillips BG, Kato M, Narkiewicz K, Choe I, Somers VK: Increases in leptin levels, sympathetic drive, and weight gain in obstructive sleep apnea. Article PubMed PubMed Central Google Scholar Mazzuca E, Battaglia S, Marrone O, Marotta AM, Castrogiovanni A, Esquinas C, Barcelò A, Barbé F, Bonsignore MR. |

Ich denke, dass Sie nicht recht sind. Ich biete es an, zu besprechen.
Und wo die Logik?