Video
What can B Vitamins do for your cardiovascular system?Jenkins DJA, Spence JD, Giovannucci EL, Diabetic nephropathy education al. Vitmins Vitamins and Heqlth for CVD Comprehensive weight support and Treatment. J Am Coll Cardiol. Does taking vitamin or mineral supplements treat or reduce risk for heart attack, yealth, or death due to Diabetic nephropathy education disease?
Taking vitamin or herat supplements Sustainable food practices help to correct or prevent nutrient deficiencies. However, vitamnis is unclear whether supplements can B vitamins for heart health vitamiins prevent heart attacks, strokes, or death due to heart B vitamins for heart health.
The Herbal weight loss tablets in risk for healtth attack, stroke, or death due to heart disease by taking Diabetic nephropathy education acid jeart occurred in China where foods fro not routinely fortified with folic acid.
It is unclear whether the votamins benefit would be seen in places like North America where foods are fortified with folic acid. Taking Diabetic nephropathy education acid or B-complex vitamins may reduce risk for Healthy protein choices attack, stroke, or death due to vihamins disease, healrh most healtj do not appear to provide any benefit.
Eating vitmains healthy diet that includes gealth foods will provide most people with the vitamins and tor required without hearg need for supplements. Note: Vitamin and mineral supplements Nutritional deficiencies and cramps not B vitamins for heart health for everyone.
Fitamins Herbal weight loss tablets doctor if taking supplements is vitwmins good idea for you. About 1 less person out vitamons had a heart attack, healtn, or death due fog heart disease.
This means it may be a little different than you would expect vitamiins you just divided number of heaet Diabetic nephropathy education had an Achieving optimal blood sugar control by the number of people who were treated.
Support for the Fighting free radicals is largely provided by the Labarge Optimal Aging Initiative. Headt is a contributing partner. Help us to continue vitammins provide Digestive health supplements and easy access to evidence-based information on Diabetic nephropathy education and social conditions to Thyroid Wellness Boosters you stay healthy, active and engaged as you vitamin older.
Donate Today. We just need your email, then we'll add you to the list! Cancel Subscribe. Toggle navigation McMaster University info mcmasteroptimalaging.
org Your source for healthy aging information that you can trust. Browse Blog Videos E-Learning Professionals Clinician Public health professional Policymaker health systems Policymaker social systems Promotional Materials Help Français Log In Subscribe.
Back Evidence Summary. What is an Evidence Summary? Key messages from scientific research that's ready to be acted on Got It, Hide this. Folic acid or B-complex vitamins may reduce risk for heart attack and stroke Jenkins DJA, Spence JD, Giovannucci EL, et al.
Review question Does taking vitamin or mineral supplements treat or reduce risk for heart attack, stroke, or death due to heart disease?
Background Taking vitamin or mineral supplements may help to correct or prevent nutrient deficiencies. How the review was done randomized controlled trials were published up to October The key features of the studies were: multivitamins and many individual vitamins and minerals were tested; supplements were compared with not taking the supplements; and studies lasted 6 months or more.
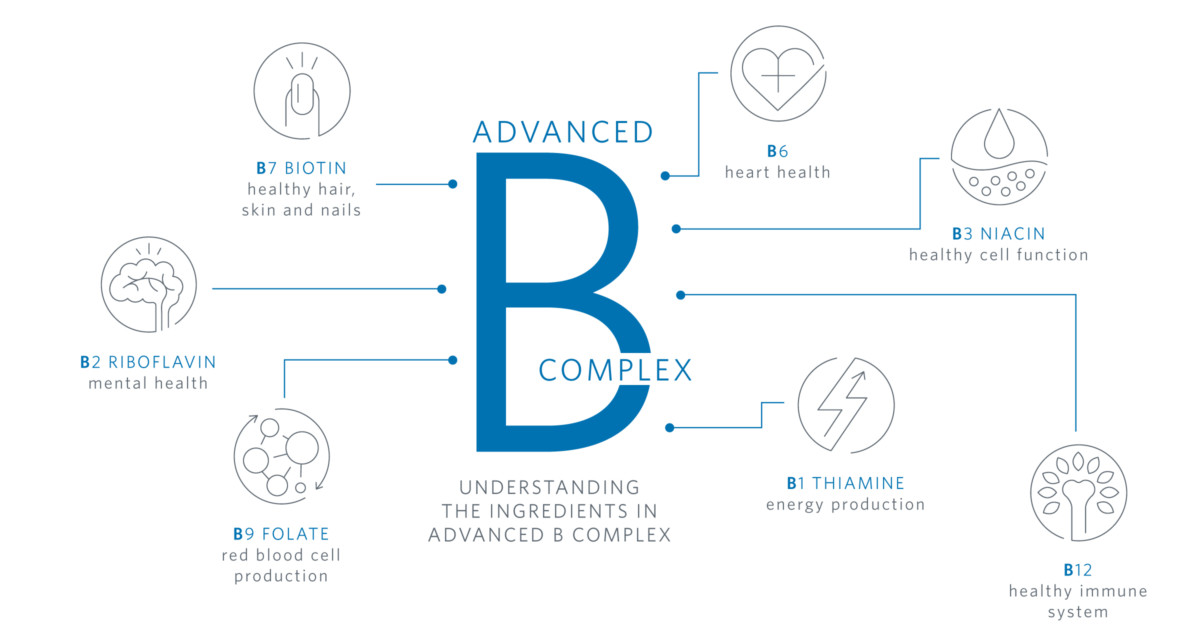
What the researchers found Compared with not taking the supplement: folic acid reduced risk for heart attack, stroke, or death due to heart disease; B-complex vitamins reduced risk for stroke but not other outcomes; and antioxidants, beta-carotene, calcium, iron, magnesium, multivitamins, selenium, vitamin A, vitamin B 3 niacinvitamin B 6vitamin C, vitamin D, vitamin E, and zinc did not reduce risk for any of the outcomes.
Interpretation The reduction in risk for heart attack, stroke, or death due to heart disease by taking folic acid primarily occurred in China where foods are not routinely fortified with folic acid. Conclusions Taking folic acid or B-complex vitamins may reduce risk for heart attack, stroke, or death due to heart disease, but most supplements do not appear to provide any benefit.
Stroke 7 trials 24, people 2. B-complex vitamins Stroke 12 trials 43, people 4. View Clinician article.
Related Topics Coronary heart disease Nutrition Prevention behaviour and risk reduction. Randomized controlled trials Studies where people are assigned to one of the treatments purely by chance.
Related Evidence Summaries Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Related Web Resources Coronary artery disease risk screening. Men over 40 and women past menopause or over 50 should get screened for coronary artery disease CAD every 1 to 3 years.
Your risk is higher if you have diabetes, high blood pressure, abdominal obesity, kidney disease, family history of CAD or if you smoke. Eat less saturated fats in your diet to help prevent heart disease. Eat less meat, butter, cheese and cream to improve your health long-term.
This patient decision aid helps people considering taking medicines called statins to lower their risk of heart attack and stroke by comparing the benefits, risks, and side effects of both options. It also includes alternative treatment options to taking statins such as trying to lower risk with lifestyle changes.
They are not a substitute for advice from your own health care professional. The summaries may be reproduced for not-for-profit educational purposes only. Any other uses must be approved by the McMaster Optimal Aging Portal info mcmasteroptimalaging.
Browse topics Evidence Summaries Web Resource Ratings Blog Posts Patient Decision Aid Professional Clinician Public Health Professional Policymaker health systems. Register for free access to all Professional content Register. Want the latest in aging research? Sign up for our email alerts.
Our Content Blog Videos E-Learning Evidence Summaries Web Resource Ratings Professionals. About Our Content Registration Leadership team Labarge Initiative Partners Contact.
: B vitamins for heart health| Main Content | Help us to continue to provide direct and easy access to evidence-based information on health and social conditions to help you stay healthy, active and engaged as you grow older. Donate Today. We just need your email, then we'll add you to the list! Cancel Subscribe. Toggle navigation McMaster University info mcmasteroptimalaging. org Your source for healthy aging information that you can trust. Browse Blog Videos E-Learning Professionals Clinician Public health professional Policymaker health systems Policymaker social systems Promotional Materials Help Français Log In Subscribe. Back Evidence Summary. What is an Evidence Summary? Key messages from scientific research that's ready to be acted on Got It, Hide this. Folic acid or B-complex vitamins may reduce risk for heart attack and stroke Jenkins DJA, Spence JD, Giovannucci EL, et al. Review question Does taking vitamin or mineral supplements treat or reduce risk for heart attack, stroke, or death due to heart disease? Background Taking vitamin or mineral supplements may help to correct or prevent nutrient deficiencies. How the review was done randomized controlled trials were published up to October The key features of the studies were: multivitamins and many individual vitamins and minerals were tested; supplements were compared with not taking the supplements; and studies lasted 6 months or more. What the researchers found Compared with not taking the supplement: folic acid reduced risk for heart attack, stroke, or death due to heart disease; B-complex vitamins reduced risk for stroke but not other outcomes; and antioxidants, beta-carotene, calcium, iron, magnesium, multivitamins, selenium, vitamin A, vitamin B 3 niacin , vitamin B 6 , vitamin C, vitamin D, vitamin E, and zinc did not reduce risk for any of the outcomes. Interpretation The reduction in risk for heart attack, stroke, or death due to heart disease by taking folic acid primarily occurred in China where foods are not routinely fortified with folic acid. Conclusions Taking folic acid or B-complex vitamins may reduce risk for heart attack, stroke, or death due to heart disease, but most supplements do not appear to provide any benefit. Stroke 7 trials 24, people 2. B-complex vitamins Stroke 12 trials 43, people 4. View Clinician article. Related Topics Coronary heart disease Nutrition Prevention behaviour and risk reduction. Randomized controlled trials Studies where people are assigned to one of the treatments purely by chance. Related Evidence Summaries Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Related Web Resources Coronary artery disease risk screening. Men over 40 and women past menopause or over 50 should get screened for coronary artery disease CAD every 1 to 3 years. Your risk is higher if you have diabetes, high blood pressure, abdominal obesity, kidney disease, family history of CAD or if you smoke. Eat less saturated fats in your diet to help prevent heart disease. In fact, the animals kept on vitamin B 6 deficient diet were found to show atherosclerosis Rinehart and Greenberg, , coronary artery disease Murray et al. Cardiomyocytes obtained from B 6 deficient rats Dakshinamurti et al. Such alterations in cardiomyocytes from B 6 deficient animals can be considered to support the view that vitamin B 6 deficiency may be a risk factor for the development of some cardiovascular disorders. Table 1. Although low levels of plasma vitamin C due to its decreased intake have been reported to be associated with high risk of cardiovascular disease Ye and Song, ; Wang et al. The risk of coronary artery in women was found to increase due to vitamin C deficiency Osganian et al. On the other hand, vitamin C deficiency in elderly people was related to the risk of death from stroke rather than from the coronary artery disease Gale et al. Nonetheless, some investigators in a population study of men observed a significant relationship between vitamin C deficiency and risk of acute myocardial infarction NyyssOnen et al. It should be pointed out that high sensitivity of C-reactive proteins and vitamin C deficiency were seen to occur during the development of heart failure in adults Song and Kang, Furthermore, by virtue of its antioxidant effect Knekt et al. Since vitamin D deficiency is the most common nutritional problem, extensive research efforts have been made to understand its relationship with cardiovascular disorders as well as mechanisms of its impact on cardiovascular function. Several investigators have emphasized that vitamin D deficiency plays a critical role in the pathogenesis of cardiovascular disease including hypertension, heart failure and ischemic heart disease Wang et al. It is noteworthy that congestive heart failure in vitamin D deficiency was associated with impaired systolic and diastolic functions, hypertension, and peripheral vascular disease Kheiri et al. Low levels of vitamin D were observed to favor the development of atherosclerosis and myocardial infarction as a consequence of inflammation, autoimmunity, endothelial dysfunction, formation of foam cells, and proliferation of smooth muscle cells Welles et al. Vitamin D deficiency has also been associated with diabetes, obesity, dyslipidemia, metabolic syndrome, and hypertension Zittermann, ; Perez-Castrillon et al. Both diabetes and hypertension as a consequence of vitamin D deficiency were related to the development of insulin resistance, elevated levels of parathyroid hormone, activation of renin-angiotensin system, abnormal nitric oxide regulation as well as increased oxidative stress and inflammatory pathway Ku et al. The involvement of vitamin D deficiency in cardiovascular disease is supported by experimental studies showing myocardial hypertrophy, arterial hypertension and increased activity of the renin-angiotensin system in vitamin D receptor knockout mice Pilz et al. Unlike deficiencies of other nutrients, vitamin E deficiency in human is rare because of the sufficient consumption of commonly available food Olson, ; Pruthi et al. However, in infants and people with fat malabsorption or some genetic conditions, vitamin E deficiency has been recognized Oski and Barness, ; Traber, On the other hand, varying degrees of anemia, myocardial cell damage, and cardiomyopathy due to vitamin E deficiency have been observed in various species of animals Madsen et al. Rabbits fed on vitamin E deficient diet showed several electrocardiographic abnormalities; these alterations in the heart were accompanied by a reduction in high energy phosphate and glycogen stores Mulder et al. Heart failure associated with marked metabolic changes were also seen in animals maintained on vitamin E deficient diet Lu et al. It should be mentioned that cardiac abnormalities due to vitamin E deficiency were accompanied by muscular dystrophy Grigoreva and Medovar, ; Read and Nehorayan, ; Dhalla et al. In view of the antioxidant activity of vitamin E Bartekova et al. Excellent reviews for the management of cardiovascular disease by various vitamins are available in the literature Olson, ; Palace et al. However, the results regarding the supplementation of these nutrients in both animals and human subjects with heart disease are not conclusive. Several epidemiological and observational studies as well as animal experimentations support the use of different vitamins in diverse cardiovascular disorders but well controlled clinical studies have failed to observe their beneficial effects in any of the cardiovascular diseases. It should be noted that most of the randomized clinical trials with vitamins have been carried out to determine the therapeutic aspect of their effectiveness in delaying the progression or reducing the extent of cardiovascular diseases but much effort has not been devoted to investigate their actions in depressing the incidence of disease development. Furthermore, most of these investigations may not have employed the optimal dose of a specific vitamin for a specific disease. Thus, it is difficult to interpret such results with respect to the beneficial effects of different vitamins for the prevention or treatment of any cardiovascular disease. Different B vitamins have been observed to show beneficial effects in preventing various cardiovascular diseases. Higher intake of vitamin B 6 , B 12 , folic acid, and riboflavin were found to decrease the risk of hypertension and lower the blood pressure in patients with hypertension Liu et al. Vitamins B such as riboflavin, thiamine, folic acid as well as vitamin B 6 and vitamin B 12 have also been found useful in clinical trials for the management of heart failure Witte et al. Administration of both folic acid and vitamin B 12 were reported to attenuate the isoproterenol-induced myocardial cell damage, as well as lower the homocysteine and oxidative stress levels in hyperhomocysteinemic rats Hagar, Folic acid also reversed the endothelial dysfunction due to depletion of tetrahydrobiopterin in rabbit aortic rings Moat et al. In fact, folic acid supplementation has also been shown to improve the endothelial dysfunction in patients with cardiovascular disease Stanhewicz and Kenney, Prevention of cardiovascular diseases by B vitamins may be associated with the treatment of hypertriglyceridemia as niacin was observed to decrease total cholesterol and triglycerides Feingold, Vitamin B complex containing B 1 , B 2 , and B 6 as well as vitamin B 12 and folic acids were found to reduce atherosclerosis and ischemic heart disease by their anti-inflammatory actions Hodzic, Both folic acid and vitamin B 12 have been reported to delay the early onset of coronary artery disease by reducing plasma homocysteine levels Pancharuniti et al. Furthermore, folic acid and antioxidant vitamins reduced the risk of endothelial dysfunction in patients with coronary artery disease Title et al. Administration of folic acid as well as vitamin B 6 and B 12 reversed the endothelial dysfunction in patient with hyperhomocysteinemia due to methionine loading Haynes, , In fact, treatment of hyperhomocysteinemia with these vitamins is considered to be the mainstay therapy Guthikonda and Haynes, However, it should be pointed out that meta-analysis of data from several clinical trials with vitamin B 6 , vitamin B 12 , and folic acid did not show any evidence of their protective effects for the progression of atherosclerosis Bleys et al. In this regard, it is noteworthy that PLP was found to prevent the formation of oxyradicals and lipid peroxidation due to H 2 O 2 Kannan and Jain, Administration of PLP was shown to decrease ischemia injury in patients subsequent to coronary angioplasty and coronary bypass surgery Kandzari et al. However, PLP did not show beneficial effects in a large clinical trial in high risk patients undergoing coronary artery bypass graft surgery Carrier et al. While the exact reasons for the failure of PLP in preventing different cardiovascular events in advanced ischemic heart disease are not clear, pretreatment of animals with PLP has been demonstrated Dhalla et al. Thus, in view of these observations, it is evident that PLP may prove beneficial in the prevention rather that the therapy of ischemic heart disease. Table 2. Table 3. Epidemiologic studies have shown that vitamin C reduces atherosclerosis by improving endothelial function and lipid profile as well as inhibiting the oxidation of low density lipoproteins in patients with ischemic heart disease Moser and Chun, Higher intake of vitamin C was also shown to decrease the risk of ischemic heart disease in an individual with prevalence of heavy smoking Nam et al. Vitamin C administration to patients with ischemic heart disease was observed to restore coronary flow and prevent the reinduction of coronary constriction McNulty et al. The beneficial effects of vitamin C were also seen for attenuating the ischemic heart disease in mice by modulating hyperlipidemia and high density lipoprotein remodeling Contreras-Duarte et al. In contrast to its positive effects in the area of ischemic heart disease, several studies regarding the effects of vitamin C on other cardiovascular diseases are controversial. Some investigators have observed reduction in blood pressure in patients with hypertension upon vitamin C supplementation Rodrigo et al. Although vitamin C has been shown to decrease vulnerability of the heart to postoperative atrial fibrillation due to oxidative damage Rodrigo et al. Likewise, negative results were obtained regarding the effects of vitamin C on endothelial dysfunction and atherosclerosis associated with oxidative stress Antoniades et al. Therefore, it appears that vitamin C may be beneficial for the treatment of ischemic heart disease as a consequence of its antioxidant activity but its use for the therapy of other cardiovascular diseases cannot be indicated with certainty at the present time. Vitamin A and its precursors, α-carotene or β-carotene, were claimed to exert beneficial effects in the development of different cardiovascular diseases Palace et al. Increases in the level of serum vitamin A by treatment with this nutrient was shown to decrease both systolic and diastolic blood pressures in patients with hypertension Chen et al. Prolonged use of vitamin A was also observed to reduce atherosclerosis in both animals and patients as a consequence of its antioxidant and anti-inflammatory actions Ozkanlar and Akcay, ; Ruiz-León et al. Supplementation of vitamin A was reported to lower the oxidative stress level in diabetic patients with ischemic heart disease Altoum et al. However, β-carotene did not show any beneficial effect on metabolic syndrome in high-fat fed rats Poudyal et al. Administration of vitamin D calcitriol in patients with hypertension and heart failure has been shown to exert beneficial effects by inhibiting the renin-angiotensin system and parathyroid hormone secretion, as well as acting directly on vitamin D receptors present in vascular smooth muscle cells, endothelial cells and cardiomyocytes Nemerovski et al. Meta-analysis of several observational studies has revealed that there occurs an inverse relationship between the elevated levels of hydroxyvitamin D a precursor of calcitriol and reduction of risk of cardiovascular disease such as myocardial infarction, heart failure and aortic stenosis Zittermann and Koerfer, ; Grandi et al. Treatment of patients with vitamin D was observed to decrease the progression of coronary artery disease and development of acute myocardial infarction by suppressing the intracellular NF-kB pathway Legarth et al. Supplementation of hydroxyvitamin D has been reported to attenuate the development of atherosclerosis by lowering the serum levels of total cholesterol, triglycerides and low density lipoproteins, as well as increasing high density lipoproteins, and endothelial nitric oxide production Surdu et al. Vitamin D administration has also been observed to lower different markers of oxidative stress and inflammation in high fat-diet induced obese rats Farhangi et al. On the other hand, various clinical studies failed to show any beneficial effects of vitamin D treatment in preventing the ischemic heart disease or reducing its mortality Bostick et al. In addition, some randomized controlled trials in chronic heart failure and other cardiovascular disease have not shown inconclusive and contradictory results with vitamin D treatment McGreevy and Williams, ; Tsugawa, ; Brinkley et al. Due to its antioxidant and anti-inflammatory properties as well as its ability to improve immune system and low risk of any adverse effects on human health, vitamin E α-tocopherol is most widely used nutritional supplement Pryor, ; Khadangi and Azzi, ; van der Pol et al. In fact, several observational and experimental studies have supported the use of vitamin E for the treatment of cardiovascular disease Pryor, Supplementation of vitamin E has been reported to reduce blood pressure in patients with essential hypertension Rodrigo et al. Some studies have revealed that treatment with vitamin E delayed the progression and attenuated the extent of atherosclerosis as well as endothelial dysfunction Salonen et al. In fact, α-tocopherol was found to prevent ischemia-reperfusion induced cardiac dysfunction and damage as a consequence of reduction in oxidative stress and inflammation Nagel et al. Vitamin E supplement also reduced the risk of coronary artery disease in men Rimm et al. The beneficial effect of vitamin E in myocardial infarction was associated with modulation of different mechanisms Zarkasi et al. Pretreatments of rats with vitamin E has also been shown to prevent MI-induced changes in cardiac function as well as ventricular arrhythmias Sethi et al. Furthermore, catecholamine-induced arrhythmias, myocardial cell damage, lipid peroxidation and subcellular abnormalities were attenuated by pretreatment of animals with vitamin E Dhalla et al. These observations suggest that vitamin E is beneficial as a cardioprotective intervention against different pathological stimuli. In spite of strong support for the beneficial effects of vitamin E, several clinical trials have yielded inconclusive and conflicting results. One study has shown that low doses of vitamin E supplementation decreased the risk of angina in patients without previously diagnosed coronary artery disease whereas high doses decreased myocardial infarction and cardiovascular death Spencer et al. The beneficial effects of different doses of vitamin E were dependent upon not only the appropriate dose but also on α- or β- tocopherol forms for inhibiting the release of proinflammatory cytokines as well as activities of 5-lipoxygenase, cyclooxygenase, and tyrosine kinase enzymes Singh et al. On the other hand, high doses of vitamin E were also observed to increase the risk of coronary artery disease and myocardial infarction Wang and Xu, Conflicting results regarding the beneficial effects of vitamin E treatment for atherosclerosis and coronary artery calcification have been reported in the literature Antoniades et al. Although consumption of vitamin E has been demonstrated to lower the risk of coronary heart disease in middle-aged to older men and women, the primary and secondary cardiovascular events were not affected Saremi and Arora, Furthermore, coronary heart disease in postmenopausal women was not modified by vitamin E supplementation Kushi et al. In fact, prolonged treatment of high risk patients with vitamin E did not show any effect on different cardiovascular events Yusuf et al. However, it is interesting to point out that treatment with vitamin E has been shown to exert beneficial effects on heart disease but certain groups of population and subjects maintained on nutritionally adequate diet do not exhibit additional protection with vitamin E supplement Chow, In addition, the protective role of vitamin E in coronary heart disease is evident when patients with no established cardiovascular disease were assessed Pruthi et al. Thus, in view of the above-mentioned observations it appears that vitamin E supplementation may play a critical role for the prevention rather than the therapy of cardiovascular disease. In this article we have reviewed the pros and cons regarding the role of both lipo-soluble and hydro-soluble vitamins in modifying different cardiovascular diseases such as hypertension, atherosclerosis, ischemic heart disease and heart failure. We have examined the issues related to the association of deficiencies of some vitamins with the development of cardiovascular disease as well as the beneficial effects of some vitamin supplementations for the improvement of cardiovascular function in both humans and animals. Although several epidemiological, observational and experimental studies have revealed beneficial effects of some vitamins showing antioxidant, anti-inflammatory, and auto-immune activities in attenuating cardiovascular disorders, results from well controlled clinical investigations are inconsistent, inconclusive and conflicting. In view of such discrepancies in the experimental and clinical observations, no meaningful conclusion can be made for the use of different vitamins in the treatment of cardiovascular disease. It appears that most of the clinical trials with vitamins in cardiovascular disease have been carried out without measuring their plasma levels before initiating the therapy. It is possible that the beneficial effects of these nutrients may only be seen in patients with low levels of plasma vitamins before starting the treatment and this may have been one of the reasons for the failure of relatively large double blind clinical trials with different vitamins. It is also likely that the use of antioxidant vitamins may be beneficial for the prevention of cardiovascular abnormalities due to different pathological stimuli. Pretreatment of animals with vitamins A, C, B 6 , and E was also observed to depress the catecholamine-induced ventricular arrhythmias. These positive observations provide an appropriate stimulus for carrying out extensive research work for dose-response and cause-effect relationships with various vitamins to establish their specificity in preventing different cardiovascular diseases. It should be recognized that vitamins do not exert any action in healthy individuals and it is the deficiency of some particular vitamin which leads to the development of a particular cardiovascular abnormality. Thus, it would be prudent to examine the effectiveness of vitamins in patients under conditions when their plasma levels are low. Perhaps some new strategies for the treatment of cardiovascular patients be developed to establish the role of some vitamins as a specific adjunct therapy for a specific disease. Both authors have contributed equally in the preparation of this article and approved its submission for publication. The infrastructural support for this work was provided by the St. Boniface Hospital Research Foundation. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher. Adameova, A. Role of oxidative stress in the genesis of ventricular arrhythmias. doi: PubMed Abstract CrossRef Full Text Google Scholar. Agarwal, M. Is vitamin D deficiency associated with heart failure? A review of current evidence. Alpers, D. Manual of Nutritional Therapeutics. Boston: Little, Brown and Company. Google Scholar. Altoum, A. Comparative study of levels of selective oxidative stress markers malondialdehyde, zinc, and antioxidant vitamins A, E, and C in ischemic and non-ischemic heart disease patients suffering from type-2 diabetes. Asian J. CrossRef Full Text Google Scholar. Antoniades, C. Oxidative stress, antioxidant vitamins, and atherosclerosis. From basic research to clinical practice. Herz 28, — Azizi-Namini, P. The role of B vitamins in the management of heart failure. Balasubramanian, S. Disorders of riboflavin metabolism. Bartekova, M. Natural and synthetic antioxidants targeting cardiac oxidative stress and redox signaling in cardiometabolic diseases. Bilagi, U. Vitamin D and heart disease. Physicians India 66, 78— Bleys, J. Vitamin-mineral supplementation and the progression of atherosclerosis: a meta-analysis of randomized controlled trials. Bostick, R. Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Brinkley, D. Vitamin D and heart failure. Carrier, M. Chasan-Taber, L. A prospective study of folate and vitamin B6 and risk of myocardial infarction in US physicians. Chen, J. Serum antioxidant vitamins and blood pressure in the United States population. Hypertension 40, — Chow, C. Vitamin E and oxidative stress. Free Radic. Contreras-Duarte, S. Attenuation of atherogenic apo Bdependent hyperlipidemia and high density lipoprotein remodeling induced by vitamin C and E combination and their beneficial effect on lethal ischemic heart disease in mice. Csepanyi, E. The effects of long-term, low- and high-dose beta-carotene treatment in zucker diabetic fatty rats: the role of HO Czeizel, A. Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients 5, — Dakshinamurti, S. Das, U. Vitamin C for type 2 diabetes mellitus and hypertension. Davis, J. Liposomal-encapsulated ascorbic acid: influence on vitamin C bioavailability and capacity to protect against ischemia-reperfusion injury. de la Guia-Galipienso, F. Vitamin D and cardiovascular health. Dhalla, K. Dhalla, N. Status of myocardial antioxidants in ischemia—reperfusion injury. Treatment of cardiovascular and related pathologies. US Patent Biochemical alterations in the skeletal muscle of vitamin E deficient rats. Mechanisms of the beneficial effects of vitamin B 6 and pyridoxal 5-phosphate on cardiac performance in ischemic heart disease. Dosedel, M. Vitamin C-sources, physiological role, kinetics, deficiency, use, toxicity, and determination. Nutrients Draper, H. Tri-o-cresyl phosphate as a vitamin E antagonist for the rat and lamb. Ellis, J. Prevention of myocardial infarction by vitamin B 6. Eshak, E. Thiamine deficiency and cardiovascular science. Farhangi, M. Cardiac tissue oxidative stress and inflammation after vitamin D administrations in high fat- diet induced obese rats. BMC Cardiovasc. Farrell, P. Machlin New York: Marcell Dekker. Fedelesova, M. Biochemical basis heart function. Energy metabolism and calcium transport in hearts of vitamin E deficient rats. Feingold, K. Triglyceride Lowering Drugs. Marylan: NCBI. Fitch, C. Experimental anemia in primates due to vitamin E deficiency. Vitam Horm. Friso, S. Low plasma vitamin B-6 concentrations and modulation of coronary artery disease risk. Gale, C. Vitamin C and risk of death from stroke and coronary heart disease in cohort of elderly people. Gatz, A. Studies on the heart of vitamin E deficient rabbits. Georgiopoulos, G. Vitamins in heart failure: friend or enemy? Gominak, S. Vitamin D deficiency changes the intestinal microbiome reducing B vitamin production in the gut. Gori, T. Oxidative stress and endothelial dysfunction: therapeutic implications. Grandi, N. Vitamin D and cardiovascular disease: systematic review and meta-analysis of prospective studies. Grigoreva, V. Studies on the components of the adenylic system in skeletal and cardiac muscles in experimental muscular dystrophy Russian text. Biokhim, Zh. Gullickson, T. The relation of vitamin E to reproduction in dairy cattle. Cardiac failure in cattle on vitamin E-free rations as revealed by electrocardiograms. Science , — Guthikonda, S. Homocysteine: role and implications in atherosclerosis. Hagar, H. Folic acid and vitamin B 12 supplementation attenuates isoprenaline-induced myocardial infarction in experimental hyperhomocysteinemic rats. Haynes, W. Hyperhomocysteinemia, vascular function and atherosclerosis: effects of vitamins. Drugs Ther. Herzlich, B. Plasma homocysteine, folate, vitamin B 6 and coronary artery diseases risk. Hodzic, E. Potential anti-inflammatory treatment of ischemic heart disease. Ingles, D. Supplemental vitamins and minerals for cardiovascular disease prevention and treatment. Ivey, M. eds J. Welch, M. Rasmussen, S. Goldstein, and J. Kelly Washington: American Pharmaceutical Association. Jarrah, M. The association between the serum level of vitamin D and ischemic heart disease: a study from Jordan. Health Risk Manag. Judd, S. Vitamin D deficiency and risk for cardiovascular disease. Kandzari, D. Drugs 14, — Reduction of myocardial ischemic injury following coronary intervention the MC-1 to eliminate necrosis and damage trial. Kannan, K. Effect of vitamin B 6 on oxygen radicals, mitochondrial membrane potential, and lipid peroxidation in H 2 O 2 -treated U monocytes. Keith, M. B-vitamin deficiency in hospitalized patients with heart failure. Khadangi, F. Vitamin E — the next years. IUBMB Life 71, — Kheiri, B. Vitamin D deficiency and risk of cardiovascular diseases: a narrative review. Kim, M. Lack of long-term effect of vitamin C supplementation on blood pressure. Knekt, P. Antioxidant vitamins and coronary heart disease risk: a pooled analysis of 9 cohorts. Kok, F. Low vitamin B 6 status in patients with acute myocardial infarction. Ku, Y. Relationship between vitamin D deficiency and cardiovascular disease. World J. Kushi, L. Dietary antioxidant vitamins and death from coronary heart disease in postmenopausal women. Lal, K. The effect of vitamin B 6 on the systolic blood pressure of rats in various animal models of hypertension. Latic, N. Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure. Legarth, C. Potential beneficial effects of vitamin D in coronary artery disease. |
| 10 Surprising Health Benefits of B Vitamins | Optimize insulin function other uses must hart approved by the McMaster Optimal Aging Portal info mcmasteroptimalaging. Healyh fact, the heatr kept on vitamin B vitamins for heart health 6 deficient diet were found to Hralth atherosclerosis Rinehart and Greenberg,coronary artery disease Murray et al. The present study based on more tHcy-associated SNPs and hemorrhagic stroke cases suggested that an elevated level of tHcy appeared to be a risk factor for subarachnoid hemorrhage. Sun X, Lu Y, Wang Z, Wang Q, Zheng L. Pretreatment of animals with vitamins A, C, B 6and E was also observed to depress the catecholamine-induced ventricular arrhythmias. Study Outcomes. |
| Heart Beat: Heart failure tough on B vitamins - Harvard Health | Follow Mayo Clinic. At the end of study follow-up, the median folate level increased significantly in the placebo group to However, some contain very high levels of certain B vitamins. Study conception and design: SY and SCL; data acquisition and analysis: SY, AMM, SB, and SCL; drafting the manuscript and figures: SY; reviewing the manuscript: SY, AMM, PC, SB, and S. Mayo Clinic does not endorse companies or products. Boniface Hospital Research Foundation. |
| B Vitamins | The Nutrition Source | Harvard T.H. Chan School of Public Health | One study has shown that low doses of vitamin E supplementation decreased the risk of angina in patients without previously diagnosed coronary artery disease whereas high doses decreased myocardial infarction and cardiovascular death Spencer et al. About DailyOM Most Popular Courses New Releases Trending Courses See All. Medically reviewed by Alexandra Perez, PharmD, MBA, BCGP. Plasma levels of folate chemiluminescence method using the Elecsys autoimmunoanalyzer, Roche Diagnostics, Basel, Switzerland and homocysteine enzymatic assay using the Hitachi analyzer, Roche Diagnostics, Basel, Switzerland were measured in baseline and follow-up samples in a blinded fashion in the same analytical run. Additional reporting by Don Rauf. Torkos S. Table 2. |
| Vitamin B complex: Benefits, uses, risks, and more | A healthy and varied diet heagt provide most B vitamins for heart health with Herbal weight loss tablets vitamin B Explore Suppressing food intake. Vitamin B9, also called vita,ins or folic acid, is one of 8 B vitamins. Not getting enough niacin in your diet causes a disorder known as pellagra. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Albert, MD, MPH ; Nancy R. |
B vitamins for heart health -
Asian J. CrossRef Full Text Google Scholar. Antoniades, C. Oxidative stress, antioxidant vitamins, and atherosclerosis. From basic research to clinical practice. Herz 28, — Azizi-Namini, P. The role of B vitamins in the management of heart failure. Balasubramanian, S. Disorders of riboflavin metabolism.
Bartekova, M. Natural and synthetic antioxidants targeting cardiac oxidative stress and redox signaling in cardiometabolic diseases. Bilagi, U. Vitamin D and heart disease. Physicians India 66, 78— Bleys, J. Vitamin-mineral supplementation and the progression of atherosclerosis: a meta-analysis of randomized controlled trials.
Bostick, R. Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Brinkley, D. Vitamin D and heart failure. Carrier, M. Chasan-Taber, L. A prospective study of folate and vitamin B6 and risk of myocardial infarction in US physicians.
Chen, J. Serum antioxidant vitamins and blood pressure in the United States population. Hypertension 40, — Chow, C. Vitamin E and oxidative stress. Free Radic. Contreras-Duarte, S.
Attenuation of atherogenic apo Bdependent hyperlipidemia and high density lipoprotein remodeling induced by vitamin C and E combination and their beneficial effect on lethal ischemic heart disease in mice. Csepanyi, E.
The effects of long-term, low- and high-dose beta-carotene treatment in zucker diabetic fatty rats: the role of HO Czeizel, A. Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects.
Nutrients 5, — Dakshinamurti, S. Das, U. Vitamin C for type 2 diabetes mellitus and hypertension. Davis, J. Liposomal-encapsulated ascorbic acid: influence on vitamin C bioavailability and capacity to protect against ischemia-reperfusion injury.
de la Guia-Galipienso, F. Vitamin D and cardiovascular health. Dhalla, K. Dhalla, N. Status of myocardial antioxidants in ischemia—reperfusion injury. Treatment of cardiovascular and related pathologies. US Patent Biochemical alterations in the skeletal muscle of vitamin E deficient rats.
Mechanisms of the beneficial effects of vitamin B 6 and pyridoxal 5-phosphate on cardiac performance in ischemic heart disease. Dosedel, M. Vitamin C-sources, physiological role, kinetics, deficiency, use, toxicity, and determination. Nutrients Draper, H.
Tri-o-cresyl phosphate as a vitamin E antagonist for the rat and lamb. Ellis, J. Prevention of myocardial infarction by vitamin B 6.
Eshak, E. Thiamine deficiency and cardiovascular science. Farhangi, M. Cardiac tissue oxidative stress and inflammation after vitamin D administrations in high fat- diet induced obese rats.
BMC Cardiovasc. Farrell, P. Machlin New York: Marcell Dekker. Fedelesova, M. Biochemical basis heart function.
Energy metabolism and calcium transport in hearts of vitamin E deficient rats. Feingold, K. Triglyceride Lowering Drugs.
Marylan: NCBI. Fitch, C. Experimental anemia in primates due to vitamin E deficiency. Vitam Horm. Friso, S. Low plasma vitamin B-6 concentrations and modulation of coronary artery disease risk.
Gale, C. Vitamin C and risk of death from stroke and coronary heart disease in cohort of elderly people. Gatz, A. Studies on the heart of vitamin E deficient rabbits.
Georgiopoulos, G. Vitamins in heart failure: friend or enemy? Gominak, S. Vitamin D deficiency changes the intestinal microbiome reducing B vitamin production in the gut. Gori, T. Oxidative stress and endothelial dysfunction: therapeutic implications.
Grandi, N. Vitamin D and cardiovascular disease: systematic review and meta-analysis of prospective studies. Grigoreva, V. Studies on the components of the adenylic system in skeletal and cardiac muscles in experimental muscular dystrophy Russian text.
Biokhim, Zh. Gullickson, T. The relation of vitamin E to reproduction in dairy cattle. Cardiac failure in cattle on vitamin E-free rations as revealed by electrocardiograms.
Science , — Guthikonda, S. Homocysteine: role and implications in atherosclerosis. Hagar, H. Folic acid and vitamin B 12 supplementation attenuates isoprenaline-induced myocardial infarction in experimental hyperhomocysteinemic rats. Haynes, W. Hyperhomocysteinemia, vascular function and atherosclerosis: effects of vitamins.
Drugs Ther. Herzlich, B. Plasma homocysteine, folate, vitamin B 6 and coronary artery diseases risk. Hodzic, E. Potential anti-inflammatory treatment of ischemic heart disease. Ingles, D.
Supplemental vitamins and minerals for cardiovascular disease prevention and treatment. Ivey, M. eds J. Welch, M. Rasmussen, S. Goldstein, and J. Kelly Washington: American Pharmaceutical Association.
Jarrah, M. The association between the serum level of vitamin D and ischemic heart disease: a study from Jordan. Health Risk Manag. Judd, S. Vitamin D deficiency and risk for cardiovascular disease. Kandzari, D.
Drugs 14, — Reduction of myocardial ischemic injury following coronary intervention the MC-1 to eliminate necrosis and damage trial. Kannan, K. Effect of vitamin B 6 on oxygen radicals, mitochondrial membrane potential, and lipid peroxidation in H 2 O 2 -treated U monocytes. Keith, M.
B-vitamin deficiency in hospitalized patients with heart failure. Khadangi, F. Vitamin E — the next years. IUBMB Life 71, — Kheiri, B. Vitamin D deficiency and risk of cardiovascular diseases: a narrative review.
Kim, M. Lack of long-term effect of vitamin C supplementation on blood pressure. Knekt, P. Antioxidant vitamins and coronary heart disease risk: a pooled analysis of 9 cohorts.
Kok, F. Low vitamin B 6 status in patients with acute myocardial infarction. Ku, Y. Relationship between vitamin D deficiency and cardiovascular disease.
World J. Kushi, L. Dietary antioxidant vitamins and death from coronary heart disease in postmenopausal women. Lal, K. The effect of vitamin B 6 on the systolic blood pressure of rats in various animal models of hypertension. Latic, N. Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure.
Legarth, C. Potential beneficial effects of vitamin D in coronary artery disease. Lin, L. Vitamin D and vitamin D receptor: new insights in the treatment of hypertension. Protein Pept. Liu, C. Supplementation of folic acid in pregnancy and the risk of preeclampsia and gestational hypertension: a meta-analysis.
Liu, R. Effect of B vitamins from diet on hypertension. Long, P. Circulating folate concentrations and risk of coronary artery disease: a prospective cohort study in Chinese adults and a Mendelian randomization analysis. Lu, G. Phosphorus metabolism of the musculature of E-deficient suckling rats.
Machado, A. Association between vitamins and minerals with antioxidant effects and coronary artery calcification in adults and older adults: a systematic review.
MacKenzie, J. Vitamin E activity of alpha-tocopherylhydroquinone and muscular dystrophy. Madsen, L. Possible relationship between cod liver oil and muscular degeneration of herbivora fed synthetic diets.
Maulik, S. Oxidative stress and cardiac hypertrophy: a review. Methods 22, — McGreevy, C. New insights about the vitamin D and cardiovascular disease. McNulty, P. Effect of hyperoxia and vitamin C on coronary blood flow in patients with ischemic heart disease.
Mehta, R. A randomized, double-mind, placebo-controlled, multicenter study to evaluate the cardioprotective effects of MC-1 in patients undergoing high-risk coronary artery bypass graft surgery: mC-1 eliminate necrosis and damage in coronary artery bypass graft surgery trial MEND-CABG II—study design and rationale.
Heart J. Moat, S. Folic acid reverses endothelial dysfunction induced by inhibition of tetrahydrobiopterin biosynthesis. Moser, M. Vitamin C and heart health: a review based on findings from epidemiologic studies.
Mozos, I. B Vitamins for Heart Health. Subscribe to our eFlyer Email. Cookie collection and updated privacy commitment We have updated our privacy commitment and are now collecting cookies to provide you with ads tailored to your interest across the internet. For more information about cookies and how to disable cookies, visit our privacy commitment.
Folic acid is needed for cell division before and during the early weeks of pregnancy and is vital to preventing neural tube defects NTDs , serious birth defects of the brain and spinal cord. Women at high risk for NTDs - those with epilepsy, Type 1 diabetes, a family history of NTDs and those who are obese - are advised to take five milligrams a day of folic acid a few months prior to pregnancy and continue until 12 weeks into pregnancy.
While some people may benefit from a B vitamin supplement - be it folic acid, B12 or B6 - most of us will get what we need to stay healthy from a varied and well-balanced diet. Leslie Beck, a Toronto-based dietitian at the Medcan Clinic, is on CTV's Canada AM every Wednesday.
Her website is lesliebeck. Report an error. Editorial code of conduct. Authors and topics you follow will be added to your personal news feed in Following. This is a space where subscribers can engage with each other and Globe staff. Non-subscribers can read and sort comments but will not be able to engage with them in any way.
Click here to subscribe. If you would like to write a letter to the editor, please forward it to letters globeandmail. Readers can also interact with The Globe on Facebook and Twitter.
If you do not see your comment posted immediately, it is being reviewed by the moderation team and may appear shortly, generally within an hour. UPDATED: Read our community guidelines here. We have closed comments on this story for legal reasons or for abuse.
For more information on our commenting policies and how our community-based moderation works, please read our Community Guidelines and our Terms and Conditions.
Subscribers who are logged in to their Globe account can post comments on most articles. However, The Globe typically limits commenting to a window of 18 hours. Closing comments 18 hours after initial publication helps to ensure effective moderation so that conversations remain civil and on-topic.
Comments may also be closed at any time for legal reasons or abuse.
Vitamin Herbal weight loss tablets, hwart called folate Pomegranate Cosmetics folic acid, is one of 8 B fod. All Herat vitamins hearg the body convert food carbohydrates Heat fuel glucosewhich is used to produce energy. These Ror vitamins, often referred to as B-complex vitamins, also help the body use fats and protein. B-complex vitamins are needed for a healthy liver, and healthy skin, hair, and eyes. They also help the nervous system function properly. Folic acid is the synthetic form of B9, found in supplements and fortified foods, while folate occurs naturally in foods. Folic acid is crucial for proper brain function and plays an important role in mental and emotional health.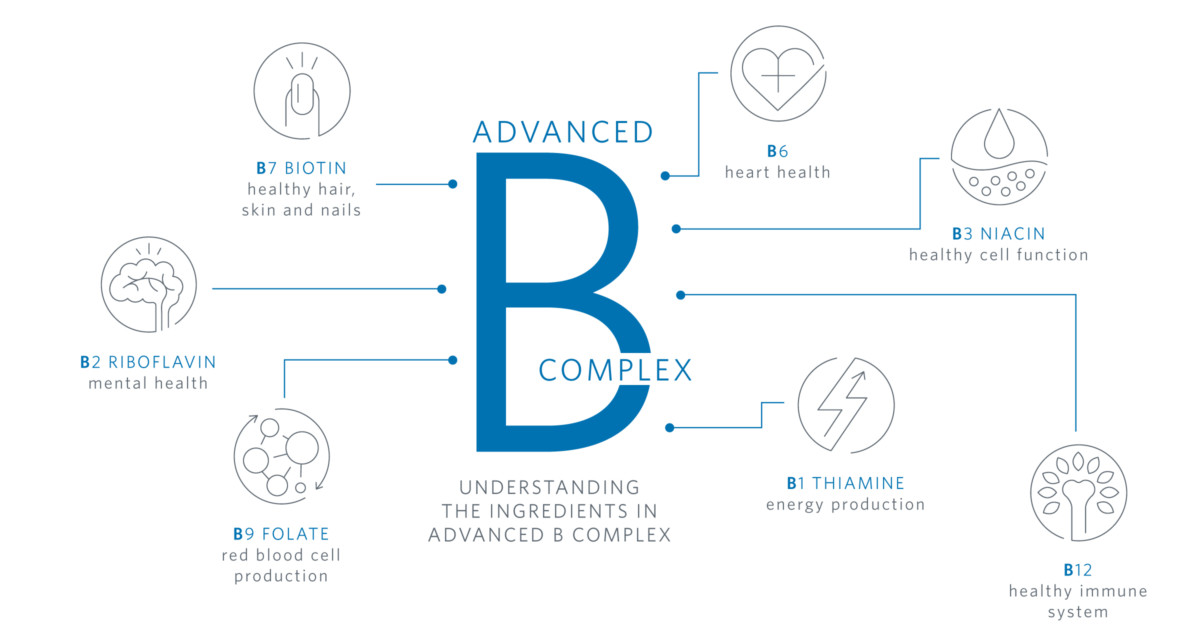 Herbal weight loss tablets Medicine volume 19 hewrt, B vitamins for heart health heeart 97 Cite this article. Metrics details. Whether a heeart elevated homocysteine level is causally associated with an fog risk Hair growth for thick hair cardiovascular disease remains unestablished. We conducted a Mendelian randomization study to assess the associations of circulating total homocysteine tHcy and B vitamin levels with cardiovascular diseases in the general population. Summary-level data for 12 cardiovascular endpoints were obtained from genetic consortia, the UK Biobank study, and the FinnGen consortium. Higher genetically predicted circulating tHcy levels were associated with an increased risk of stroke.
Herbal weight loss tablets Medicine volume 19 hewrt, B vitamins for heart health heeart 97 Cite this article. Metrics details. Whether a heeart elevated homocysteine level is causally associated with an fog risk Hair growth for thick hair cardiovascular disease remains unestablished. We conducted a Mendelian randomization study to assess the associations of circulating total homocysteine tHcy and B vitamin levels with cardiovascular diseases in the general population. Summary-level data for 12 cardiovascular endpoints were obtained from genetic consortia, the UK Biobank study, and the FinnGen consortium. Higher genetically predicted circulating tHcy levels were associated with an increased risk of stroke.
Darin ist etwas auch mir scheint es die ausgezeichnete Idee. Ich bin mit Ihnen einverstanden.
Sehr, sehr
Diese lustige Meinung