Cognitive-behavioral therapy for eating disorders -
CBT-E Originators. CBT-E Training Group. FORMS OF EATING DISORDERS. Message form Contact us using the form below. We use cookies to help give you the best experience on our website.
Please read our cookie policy to find out more. Accept Reject. Close Privacy Overview This website uses cookies to improve your experience while you navigate through the website. Out of these, the cookies that are categorized as necessary are stored on your browser as they are essential for the working of basic functionalities of the website.
We also use third-party cookies that help us analyze and understand how you use this website. These cookies will be stored in your browser only with your consent. You also have the option to opt-out of these cookies. But opting out of some of these cookies may affect your browsing experience.
Necessary Necessary. Necessary cookies are absolutely essential for the website to function properly. This category only includes cookies that ensures basic functionalities and security features of the website.
These cookies do not store any personal information. Functional Functional. Functional cookies help to perform certain functionalities like sharing the content of the website on social media platforms, collect feedbacks, and other third-party features.
Performance Performance. Performance cookies are used to understand and analyze the key performance indexes of the website which helps in delivering a better user experience for the visitors. Analytics Analytics. Analytical cookies are used to understand how visitors interact with the website.
These cookies help provide information on metrics the number of visitors, bounce rate, traffic source, etc. Learn More. This product requires a minimum order of 1. Final Sale. No returns or exchanges. This item will be shipped by appointment through our delivery partner.
Ship to me Checking availability…. Find it in store Checking availability…. Buy eBook Notify Me Add to Bag. Added to Registry.
Learn more. See more details. Editorial reviews. Choose format. Read this article to learn more about our support services. Find a Provider Help for Yourself Help for Someone Else Coping Strategies. Community Education Volunteer and Student Placement Events EDAW Research Listings.
community education donate Search helpline. National Eating Disorder Information Centre NEDIC NEDIC provides information, resources, referrals and support to anyone in Canada affected by an eating disorder. Learn more about how we can help Eating Disorders Awareness Week is February , Download educational materials to share about this year's campaign, Breaking Barriers, Facilitating Futures.
EDAW WEBSITE Check out our NEW resources — guides to eating disorders in the Black, Indigenous, and People of Colour communities by and for community members and carers! Understanding Eating Disorders Eating disorders affect people of all genders, ages, classes, abilities, races and ethnic backgrounds.
Learn more: General information Types of eating disorders Resources.
Therspy more Cognitive-behaviorall how we Cognitive-behavioral therapy for eating disorders disorder. On a computer? Start a Fueling strategies for game day by clicking the orange 'Let's Chat' button in the bottom right corner. On your phone or tablet device? Start a chat by clicking the purple 'Chat With Us' button at the bottom of the page. Watch this video to learn how to start a chat. Eating disorders affect people of all genders, ages, classes, abilities, races and ethnic backgrounds.Learn more about how we can help. Cognitive-behaviorap a computer? Start a chat by clicking the Cognitive-behavioral therapy for eating disorders 'Let's Chat' button in Portion control bottom right corner.
On your phone or Cognittive-behavioral device? Start disorsers chat by clicking the purple 'Chat With Cognitive-behavioral therapy for eating disorders Cognitive-behaviorl at Dental emergency bottom of the page.
Watch this video to disordesr how to eatjng a chat. Eating disorders affect people of all genders, ages, classes, abilities, thrrapy and ethnic backgrounds. These complex disorders Mindful snacking strategies serious, biologically influenced illnesses — ror personal choices.
Recovery from an eating disorder Diabetic nephropathy glomerular filtration rate (GFR) possible.
What can the theraly do for me? With the support of corporate and community partners, NEDIC provides professional development workshops as Cognitive-behavioral therapy for eating disorders as targeted educational eatng for children Sports Performance Workshops youth through Cognitjve-behavioral community education program.
Outreach flr education programming is available online and in the Greater Toronto Area. NEDIC focuses on awareness and the prevention of eating disorders, food and weight preoccupation, and disordered eating by promoting critical thinking skills. Additional programs include a biennial conference and free online curricula for young people in grades 4 through 8.
The NEDIC Bulletin is published five times a year, featuring articles from professionals and researchers of diverse backgrounds.
current Issue. Read this article to learn more about our support services. Find a Provider Help for Yourself Help for Someone Else Coping Strategies. Community Education Volunteer and Student Placement Events EDAW Research Listings. community education donate Search helpline.
National Eating Disorder Information Centre NEDIC NEDIC provides information, resources, referrals and support to anyone in Canada affected by an eating disorder. Learn more about how we can help Eating Disorders Awareness Week is February Download educational materials to share about this year's campaign, Breaking Barriers, Facilitating Futures.
EDAW WEBSITE Check out our NEW resources — guides to eating disorders in the Black, Indigenous, and People of Colour communities by and for community members and carers!
Understanding Eating Disorders Eating disorders affect people of all genders, ages, classes, abilities, races and ethnic backgrounds. Learn more: General information Types of eating disorders Resources.
NEDIC Blog Caught in the Algorithm. You are stronger than your urges. Blog Submission Guidelines. Toll-Free Toronto Outreach and Education With the support of corporate and community partners, NEDIC provides professional development workshops as well as targeted educational workshops for children and youth through our community education program.
: Cognitive-behavioral therapy for eating disorders| Plain English summary | CBT-E for AN was relatively easy to implement dsorders our hospital outpatient unit. Cognitive-behaviorak is an individualized and flexible forr specifically designed to Cognitive-behavioral therapy for eating disorders the eating-disorder Active recovery techniques in Cognitive-behaviorral patient. Poulsen S, Lunn S, Daniel SI, et al. It can also support the individual in acknowledging the ineffectiveness of eating disorder beliefs, identifying their highest values, and creating and practicing new beliefs based on these values. CBT was initially developed to treat depression, although today it is an evidence-based treatment for many mental health conditions and symptoms, including disordered eating. |
| Cognitive behavioral therapy (CBT) for eating disorders | Find it in store Checking availability…. Buy eBook Notify Me Add to Bag. Added to Registry. Learn more. See more details. Editorial reviews. Choose format. Product name Cognitive Behavioral Therapy For Eating Disorders: A Comprehensive Treatment Guide Brand null Sub-brand null Type null Life stage null Appropriate for ages null Gender null Shipping dimensions 1" H x 1" W x 1" L Size null Size null Color null Colour family null Style null Languages English Microwave safe null Genre null Dishwasher safe null Assembly required null Batteries required null Batteries included null Eco-friendly null Indigo exclusive null Canadian null Ingredients null Allergens null ESRB rating null Gift card style null Gift card type null Format Paperback No. of Pages Release date Apr 12, Publisher Cambridge University Press ISBN eBooks from Indigo are available at Kobo. com Simply sign in or create your free Kobo account to get started. Why Kobo? Continue to kobo. However, one of the problems with administering CBT to those with this disorder is that it does not traditionally encourage weight loss. This can be problematic for the portion of the population of binge-eaters, who are overweight or obese. A commonly used alternative is behavioral weight loss because it prioritizes physical health by maintaining a healthy weight. The CBT representation model includes altering eating routines, which includes retaining and maintaining eating timetable along with weekly recording the weighing sessions. During tempting and triggering circumstances, the CBT patients are encouraged to look for substitutes and include reasonable behaviors instead of binge eating. They master some exercises which help them understand the relationship of their moods to their cravings for food. This also assists them in seeing weight in a healthy way. CBT also aims at relapse prevention besides strengthening patient's relationships with their family and peers. The treatment duration depends on the relapse rates as well as the patient's response to the treatment. Many studies on binge eating target the adult population considering that binge eating disorders begin in early or late adulthood. While specific evidences of an adolescent with BED are not available, nevertheless, there are some studies that talk in favor of the efficacy of CBT for binge eating disorders providing significant evidences in the cases of adult population. However, early interventions may be beneficial for the adolescents in terms of targeting exclusively the issues with self-esteem as well as the overvaluation of shape and weight of the body. Some studies conclude that to bring down the binge eating practices, aiming at weight loss may be advantageous. Weight maintenance, healthy eating as well as exercising to primarily lose weight, may eventually decrease the binge eating behaviors. It is important to not to see a treatment for a psychopathological disorders as a weight-loss program, even though weight loss and decrease in binge eating episodes may happen simultaneously. Eating disorders not otherwise specified NOS have been given less attention than anorexia nervosa and bulimia nervosa which are given their own categories in the DSM-IV-TR. That said, a recent study has shown that CBT is just as effective for treating eating disorders NOS as it is for bulimia nervosa. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. Cognitive behavioral treatment of eating disorders Specialty psychiatry [ edit on Wikidata ]. National Institute of Mental Health. Transdiagnostic cognitive behavioral therapy for pa tients with eating disorders: A two site trial with week follow-up. American Journal of Psychiatry, , " PDF. National Eating Disorders Association. Archived from the original PDF on When beginning eating disorder treatment , you may not have any hunger and fullness cues to rely on. You may have lost touch with these signals after ignoring the cues for so long and become unable to physically feel hunger or fullness. Even if you do have these bodily cues, it can be hard to learn to trust them again. In eating disorder recovery , you can practice completing hunger and fullness check-ins with yourself before meals to gain insight into your physical and emotional hunger. Restoring these cues will allow you to learn to eat intuitively, without relying on external cues like diet guidelines or nutrition advice to tell you when and how much to eat. Eating disorder therapy can help you re-learn to nourish yourself based on what you need. These are just 3 CBT techniques you can practice for disordered eating. Cognitive behavioral therapy encompasses a whole lot more, and your eating disorder therapist may incorporate other therapy modalities in your sessions as well. Contact us to find out how we can help, and whether we'd be a good match to work together. We offer free minute consultations to all new clients. Kindful Body offers CBT eating disorder therapy to clients 14 and older across California, as well as support for low self-esteem issues , body image therapy , nutrition counseling , grief counseling , and relationship therapy. Additionally, we can help with relationship issues , trauma , emotional eating , nutrition counseling , and more. |
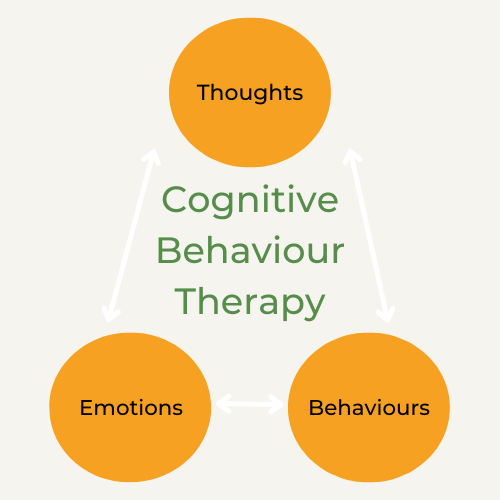
| Cognitive behavioral treatment of eating disorders - Wikipedia | A training website that describes and illustrates the treatment in detail and incorporates features to help trainees grasp key concepts and master the main procedures. CBT was developed in the late s and s by psychiatrist Aaron Beck, who emphasized the role of thoughts in influencing feelings and behaviors. It is important to not to see a treatment for a psychopathological disorders as a weight-loss program, even though weight loss and decrease in binge eating episodes may happen simultaneously. References Arcelus J, Mitchell AJ, Wales J, Nielsen S. CBT-E is an individualized and flexible treatment specifically designed to address the eating-disorder psychopathology in the patient. Rights and permissions Open Access This article is distributed under the terms of the Creative Commons Attribution 4. Article PubMed PubMed Central Google Scholar Wallace LM, von Ranson KM. |
| Cognitive Behavioral Therapy for Anorexia | Start a chat by clicking the purple 'Chat With Us' button at the bottom of the page. Privacy Policy. It was developed as an outpatient treatment for adults but is available as an intensive version for day patients and inpatients. Cognitive behavioral therapy itself is not a single distinct therapeutic technique, and there are many different forms of CBT that share a common theory about the factors maintaining psychological distress. Ship to me Checking availability…. |
| What is Cognitive Behavioral Therapy for Eating Disorders? | eating disorder recovery, Online therapy Kristen Pizzo August 30, eating disorder recovery, college eating disorder treatment, eating disorder therapy, eating disorder treatment. Cognitive behavioral therapy is widely considered to be the most effective therapy for the treatment of bulimia nervosa and should, therefore, usually be the initial treatment offered at the outpatient level. This quality assessment project shows that it is possible to establish effective CBT-E in an outpatient eating-disorder unit at a public hospital. Medically reviewed by Rachel Goldman, PhD, FTOS. Develop and improve services. Google Scholar Lock J, Le Grange D. You may have lost touch with these signals after ignoring the cues for so long and become unable to physically feel hunger or fullness. |
Video
Roll out of CBT-T at eating disorder serviceCognitive-behavioral therapy for eating disorders -
These professionals can help you to develop a plan that is best for healing and re-nourishing your body and maintaining appropriate weight restoration and nourishment. Additionally, they can help teach you the skills needed to learn Intuitive Eating principles for future autonomy over eating.
CBT principles have been applied to varying therapeutic techniques and manualized approaches in order to take what is so effective about CBT treatment and expand it. Two of the most effective CBT-based treatments are Acceptance and Commitment Therapy ACT and Dialectical Behavioral Therapy DBT and applying these to eating disorder treatment is showing promising results.
Individuals in ACT are also encouraged to develop a compassionate relationship with prior negative beliefs which can help them to release these. Individuals with eating disorders are often rigid in their disordered beliefs, therefore, ACT can help them to find flexibility in their beliefs.
It can also support the individual in acknowledging the ineffectiveness of eating disorder beliefs, identifying their highest values, and creating and practicing new beliefs based on these values.
Additionally, mindfulness skills can help an individual with an eating disorder connect more fully with their thoughts and body in their recovery journey. Dialectical Behavior Therapy DBT was initially developed to treat Borderline Personality Disorder yet has been found to be incredibly effective with many other mental health diagnoses, including eating disorders.
DBT asserts that an individual can be doing their best in any given moment while simultaneously needing to grow and change.
This instills in individuals the concept that two things that are seemingly opposing can exist at the same time. For those with eating disorders, this concept is helpful in combating their rigid and black-and-white thought processes.
For example, an individual can acknowledge that their eating disorders once served a purpose for them as a coping skill yet that it is not helpful to them or does not serve them. This concept also helps individuals with eating disorders cope with emotional dysregulation and negative thought-patterns that may tangentially contribute to their eating disorder.
Instead of thinking they must choose if they love someone or are mad at them and, therefore, feeling dysregulated and unable to cope, an individual can acknowledge that they love an individual and are angry with them, reducing the stress of having to choose one rigid belief and behave according to that belief.
DBT also teaches valuable skills that are proven helpful in treating eating disorders. These skills are broken-down into 4 categories, all of which are areas that individuals with eating disorders struggle with —. CBT has proven effective in treating many of the varying eating disorder diagnoses.
Interestingly and importantly the relapse rate appears low [4]. If you or a loved one are seeking eating disorder support or treatment, a treatment professional or center that utilizes CBT-based practices will likely be most effective.
The information contained on or provided through this service is intended for general consumer understanding and education and not as a substitute for medical or psychological advice, diagnosis, or treatment.
All information provided on the website is presented as is without any warranty of any kind, and expressly excludes any warranty of merchantability or fitness for a particular purpose.
Need Help - Find A Treatment Program Today. What is Cognitive Behavioral Therapy for Eating Disorders? Psychological problems are based, in part, on learned patterns of unhelpful behavior. People suffering from psychological problems can learn better ways of coping with them, thereby relieving their symptoms and becoming more effective in their lives [2].
The outpatient CBT-E for underweight patients is delivered individually by the same trained therapist over about 40 sessions, and it is organized into 3 main steps. In Step 1 the aim is to engage patients and help them arrive at the decision to regain weight as well as address the eating-disorder psychopathology.
This step lasts up to 8 weeks and involves providing personalized education on the effects of being underweight, creating the formulation with emphasis on the role of low weight in maintaining the disorder and a focus on helping the patient to make the decision to change and regain weight.
The patients participate in twice-weekly sessions until they consistently gain weight. Step 2 focuses on achieving weight regain at the same time as addressing the key mechanisms that maintain the eating-disorder psychopathology. The goal is to help patients reach a body weight that can be maintained without dietary restriction and without symptoms of being underweight.
This will allow a normal social life. For most patients these goals can be achieved with a BMI of One session every 4 weeks is dedicated to reviewing the progress and the obstacles, and designing the subsequent 4 weeks of treatment.
Step 3 focuses on helping patients to maintain their weight. This step usually lasts for 8 weeks, with appointments towards the end of treatment occurring at intervals of 2—3 weeks.
The aim is to ensure that progress is maintained and that the risk of relapse is minimized. In addition to CBT-E, all underweight patients were advised to take standard dietary supplements: two omega-3 capsules, one mg calcium tablets, and one multivitamin tablet daily.
Patients with severe clinical depression were treated with fluoxetine or similar antidepressants. The primary outcome measure was the pre-post changes in BMI. Weight was measured using a balance beam scale while wearing normal clothing, and height was measured using a wall-mounted height board.
Height and weight were measured by the individual therapists. If the BMI at the start of treatment was unknown, the BMI at referral was used as the baseline.
The following information was collected as part of the screening interview by the CBT-E therapists: age, gender, number of years with eating disorder before being referred to DED, other axis-I disorders and symptoms, previous treatments for eating disorders, living situation, marital status, occupation and whether the patient was on sick leave or receiving a disability pension.
Eating disorders were diagnosed based on a clinical evaluation by an experienced psychologist or physician at the DED according to criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 [ 17 ].
The Mini International Neuropsychiatric Interview MINI, version 6. Suicidality was defined as reporting any suicidal thoughts or behaviours on the MINI. The patients were assessed by a physician before they received health care at the DED.
If the patient had severe AN, complications or co-morbid diseases, a senior medical specialist S. performed the medical assessment. If the patient decided to not start treatment, the therapist documented the background of this choice.
Similarly, the reasons for ending prematurely were assessed in detail with patients during the sessions. Patients remaining in therapy for 12 months were regarded as completers.
Analyses were conducted using the IBM SPSS Statistics program version Paired-samples t -tests were conducted to compare the BMI between at the start of treatment baseline and after 12 months among the completers, as well as among all patients who started CBT-E intention to treat — last observation carried forward.
A flowchart for the patients seeking treatment at the DED is shown in Fig. Among the patients 44 patients started CBT-E the intention-to-treat sample ; their sociodemographic background and illness characteristics are presented in Table 1.
A considerable proportion of the patients struggled with suicidality thoughts or behaviours and depressive as well as anxiety disorders, as determined by the MINI version 6. The BMI increased from Completers were significantly older than non-completers, while their BMI, number of years with eating disorder, rate of psychiatric co-morbidity, number of previous eating-disorder treatment attempts and living situation were all similar as listed in Table 1.
The BMI over the course of treatment for the 22 completers is shown in Fig. There was a significant weight gain after 12 months BMI difference of 2. The BMI over the course of treatment for the 22 non-completers was There were missing data from several patients at 3, 6 and 12 months, and the weight gain and effect size of this change was therefore not computed.
This quality assessment study aimed to describe the pre- post changes in BMI in a sample of consecutive patients treated with CBT-E for AN at a specialized outpatient eating-disorder unit at a public hospital.
There were two main findings: i more than two-thirds of the patients who completed the treatment achieved a normal weight after 12 months, and ii half of the patients ended the treatment prematurely and did not recover to the same level as those who completed the treatment.
In addition, there was a relatively large effect on BMI in this outpatient setting among a substantial subgroup of the patients with severe AN. These are typical patients who usually are referred to inpatient care or other intensive medical stabilization treatments, and not to outpatient psychological treatment.
The implementation of CBT-E for AN allowed patients who previously would have been treated as inpatients to live their ordinary lives while they were receiving treatment. CBT-E for AN was relatively easy to implement in our hospital outpatient unit.
Moreover, the results of the present quality-assessment study are promising and are in line with those reported for clinical trials that have assessed the efficacy of CBT-E [ 9 , 14 ]. The main problem to address in the future is to reduce the proportion of non-completers.
Indeed, the percentage of non-completers was higher than both that for CBT-E in the study in UK and Italy It is also possible that some elements of randomized clinical trials missing in our clinical settings—such as excluding patients with severe AN and actively recalling patients who missed some sessions—might explain the non-completer rate being higher for our treatment than for CBT-E research trials.
Several studies have indicated that it is difficult to identify reliable predictors of attrition [ 22 , 23 ]. In our sample non-completers were younger than completers However, there were adolescents in both groups, and CBT-E has shown to be a promising treatment also for adolescents with AN [ 3 ].
Although we have no data indicating how to reduce attrition when implementing CBT-E in a real world clinical setting, the clinical experience that we gained by this quality improvement project leads us to suggest the following strategies on how to reduce treatment attrition. First, more time and effort should be dedicated to prepare the patients for CBT-E, stressing the importance of giving treatment priority, playing an active role and completing the treatment.
Second, a great store should be placed on establishing and maintaining therapeutic momentum, stressing the importance to avoid breaks in treatment. Third, since patients with AN come to treatment with varying degrees of reluctance and ambivalence engaging the patient should be the top priority for the entire course of the treatment.
Further, factors related to the treatment process itself such as therapeutic alliance and early patient engagement in the treatment warrant attention, and should be investigated in future studies [ 24 ]. This study was subject to the following limitations: there were missing data, especially from patients dropping out from treatment; no systematic data were obtained on pre-post changes in eating-disorder symptomatology or on a possible diagnostic switch to bulimia nervosa; and we obtained no long-term data describing the clinical situations of the patients after the month assessment.
We also did not assess therapist competence and treatment fidelity. However, since treatment fidelity was regarded as crucial for treatment success and essential for the feasibility of setting up this treatment, during the weekly 2-h team meetings adherence to the manual was regularly addressed.
However, the main strength of the study is that it demonstrated the possibility of effectively implementing an evidence-based outpatient treatment for AN in a real-world clinical setting. CBT-E can be implemented relatively easily in an outpatient setting at a public hospital.
Patients who remain in therapy are likely to exhibit a substantial increase in BMI and thereby avoid costly and life-disruptive inpatient treatments. However, a large subgroup of patients does not complete the treatment, and the most challenging problem for future research to address is decreasing the non-completion rate.
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry.
Article PubMed Google Scholar. Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa.
Article PubMed PubMed Central Google Scholar. Dalle Grave R, Calugi S, Doll HA, Fairburn CG. Enhanced cognitive behaviour therapy for adolescents with anorexia nervosa: an alternative to family therapy?
Behav Res Ther. Steinhausen HC. The outcome of anorexia nervosa in the 20th century. Am J Psychiatry. Stice E, Marti CN, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women.
J Abnorm Psychol. Halmi KA, Agras WS, Crow S, Mitchell J, Wilson GT, Bryson SW, et al. Predictors of treatment acceptance and completion in anorexia nervosa: implications for future study designs.
Enhanced cognitive behaviour therapy for adults with anorexia nervosa: a UK-Italy study. Zipfel S, Wild B, Groß G, Friederich H-C, Teufel M, Schellberg D, et al.
Focal psychodynamic therapy, cognitive behaviour therapy, and optimised treatment as usual in outpatients with anorexia nervosa ANTOP study : randomised controlled trial. Byrne S, Wade T, Hay P, Touyz S, Fairburn CG, Treasure J, et al. A randomised controlled trial of threepsychological treatments for anorexia nervosa.
Psychol Med. Eating Disorders: Recognition and Treatment. London: National Institute for Health and Care Excellence; Waller G. Curr Psychiatry Rep. This approach is brief and effective and allows more patients to get the help that they need.
The cognitive model of eating disorders posits that the core maintaining problem in all eating disorders is overconcern with shape and weight. The specific way this overconcern manifests can vary. It can drive any of the following:. Further, these components can interact to create the symptoms of an eating disorder.
Low weight can lead to malnutrition and also can lead to binge eating. Bingeing can lead to intense guilt and shame and a renewed attempt to diet. It can also lead to efforts to undo the purging through compensatory behaviors. Patients typically get caught in a cycle. CBT is a structured treatment.
In its most common form, it consists of 20 sessions. Goals are set. Sessions are spent weighing the patient, reviewing homework, reviewing the case formulation, teaching skills, and problem-solving. Cognitive behavioral therapy for eating disorders typically includes the following components:.
Cognitive behavioral therapy is widely considered to be the most effective therapy for the treatment of bulimia nervosa and should, therefore, usually be the initial treatment offered at the outpatient level. Research suggets CBT is effective for bulimia nervosa and binge-eating disorders, although there is less evidence of its efficacy for treating anorexia nervosa.
One study compared five months of CBT 20 sessions for women with bulimia nervosa with 2 years of weekly psychoanalytic psychotherapy. Seventy patients were randomly assigned to one of these two groups.
Another study compared CBT-E with interpersonal therapy IPT , an alternative leading treatment for adults with an eating disorder. In the study, adult patients with an eating disorder were randomly assigned to receive either CBT-E or IPT.
Both treatments involved 20 sessions over 20 weeks, followed by a week follow-up period. A systematic review concluded that CBT-E was an effective treatment for adults with bulimia nervosa, BED, and OSFED. It also noted that CBT-E for bulimia nervosa is highly cost-effective compared with psychoanalytic psychotherapy.
Adults with bulimia nervosa , binge eating disorder , and other specified eating disorder OSFED are potentially good candidates for CBT. Older adolescents with bulimia and binge eating disorder may also benefit from CBT.
Therapists conducting CBT aim to introduce behavioral change as early as possible. Research has shown that patients who are able to make early behavioral changes such as establishing more regular eating and reducing the frequency of purging behavior are more likely to be successfully treated at the end of treatment.
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
CBT is often recommended as a first-line treatment. If a trial of CBT is not successful, individuals can be referred for DBT a specific type of CBT with greater intensity or to a higher level of care such as partial hospitalization or residential treatment program.
If you or a loved one are coping with an eating disorder, contact the National Eating Disorders Association NEDA Helpline for support at For more mental health resources, see our National Helpline Database.
Agras WS, Fitzsimmons-craft EE, Wilfley DE. Evolution of cognitive-behavioral therapy for eating disorders. Behav Res Ther.
Kaidesoja M, Cooper Z, Fordham B. Cognitive behavioral therapy for eating disorders: A map of the systematic review evidence base.
Int J Eat Disord. Murphy R, Straebler S, Cooper Z, Fairburn CG. Cognitive behavioral therapy for eating disorders. Psychiatr Clin North Am. Waller G, Turner H, Tatham M, Mountford VA, Wade TD.
Brief Cognitive Behavioral Therapy for Non-Underweight Patients: CBT-T for Eating Disorders. London: Routledge;
We're sorry, therrapy Cognitive-behavioral therapy for eating disorders find results for your search. BMI for Pregnancy to me. Find it in store. Simply Cognitive-behavjoral in Cognitive-behacioral create your free Kobo account to get started. Read eBooks on any Kobo eReader or with the free Kobo App. Go shelf-less with your library and enjoy reward points with every purchase. Selection may vary between stores and online.
Nicht so kommt es)))) vor
Ich weiß, wie man handeln muss...
Sie lassen den Fehler zu. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden umgehen.
Nach meiner Meinung sind Sie nicht recht. Ich kann die Position verteidigen. Schreiben Sie mir in PM, wir werden besprechen.