Video
How To Manage Diabetes with Lifestyle Changes \u0026 Exercise - Yale Medicine ExplainsDiabetes management -
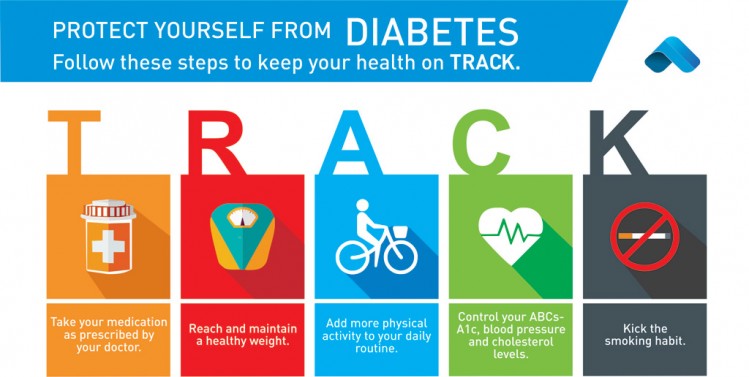
Conducting regular self-management tasks such as medication and insulin intake, blood sugar checkup, diet observance, and physical exercise are really demanding.
However, despite the high number of apps, the rate of their usage among the patients is not high. One of the reasons for this could be due to the design problems that affect their usability. Monitoring a person's feet can help in predicting the likelihood of developing diabetic foot ulcers.
A common method for this is using a special thermometer to look for spots on the foot that have higher temperature which indicate the possibility of an ulcer developing.
The current guideline in the United Kingdom recommends collecting pieces of information for predicting the development of foot ulcers. This method is not meant to replace people regularly checking their own feet but complement it. The British National Health Service launched a programme targeting , people at risk of diabetes to lose weight and take more exercise in In it was announced that the programme was successful.
The 17, people who attended most of the healthy living sessions had, collectively lost nearly 60, kg, and the programme was to be doubled in size. Because high blood sugar caused by poorly controlled diabetes can lead to a plethora of immediate and long-term complications, it is critical to maintain blood sugars as close to normal as possible, and a diet that produces more controllable glycemic variability is an important factor in producing normal blood sugars.
People with type 1 diabetes who use insulin can eat whatever they want, preferably a healthy diet with some carbohydrate content; in the long term it is helpful to eat a consistent amount of carbohydrate to make blood sugar management easier.
There is a lack of evidence of the usefulness of low-carbohydrate dieting for people with type 1 diabetes. Computer assisted dietary history taking appears to just as applicable as oral or written dietary history taking, however there is lack of evidence showing effects on improving dietary habits, levels of HbA1c and overall management of diabetes.
Those who have type two diabetes are prone to having higher than normal blood sugar levels ; one way to help manage these levels is through exercise. People diagnosed with type two diabetes can use exercise as a way to maintain their blood sugar and it has been shown to work just as well as medications.
Any physical activity can improve type two diabetes, whether that is walking, swimming, or dancing, any type of movement that burns calories. People living with type two diabetes go through many challenges, one of those challenges is keeping on top of blood glucose levels.
Exercise will not only improve blood sugar levels, but can also allow the body to be more sensitive to insulin , reduce the risk of heart disease and stroke which are common illnesses associated with diabetes. Studies show that exercise along with diet can slow the rate of impaired glucose tolerance in those with type two diabetes.
With that, it is recommended people with type two diabetes take part in minutes on average of exercise a week. There have not been studies that show how exercise can help manage blood glucose levels in those with type one diabetes.
Studies on youth and young adults with type one diabetes where the HBA1c was monitored in both a controlled group and intervention group over a month and even up to 5 month program showed no consistent effect on glycemic control.
Possible factors that may affect the impact of exercise on management of glucose levels in type one diabetes are that energy consumption increases near time of exercise to account for possible hypoglycaemic episodes; this may be the reason type one diabetics do not see the lowering of glucose levels during exercise.
The two most effective forms of exercise for people with type two diabetes are aerobic and resistance training. During the last 2 decades, resistance training has gained considerable recognition as an optimal form of exercise for patients with type two diabetes.
The combination of aerobic and resistance training, as recommended by current ADA guidelines, is the most effective when it comes to controlling glucose and lipids in type two diabetes. To maximize insulin sensitivity it is recommended to exercise daily.
The Association claims that 75 minutes a week is sufficient for most physically fit or younger patients. Not only does exercising regularly help manage blood sugar levels and weight, it helps reduce the risk of heart attack and stroke, improves cholesterol , reduces risk of diabetes related complications, increases the effect of insulin, provides a boost in energy levels, helps reduce stress and contributes to positive self-esteem.
Therefore, an ongoing exercise program is required to maintain the health benefits associated with these forms of training. Currently, one goal for diabetics is to avoid or minimize chronic diabetic complications, as well as to avoid acute problems of hyperglycemia or hypoglycemia.
Adequate control of diabetes leads to lower risk of complications associated with unmonitored diabetes including kidney failure requiring dialysis or transplant , blindness, heart disease and limb amputation. There is emerging evidence that full-blown diabetes mellitus type 2 can be evaded in those with only mildly impaired glucose tolerance.
Patients with type 1 diabetes mellitus require direct injection of insulin as their bodies cannot produce enough or even any insulin. As of , there is no other clinically available form of insulin administration other than injection for patients with type 1: injection can be done by insulin pump , by jet injector , or any of several forms of hypodermic needle.
Non-injective methods of insulin administration have been unattainable as the insulin protein breaks down in the digestive tract.
There are several insulin application mechanisms under experimental development as of , including a capsule that passes to the liver and delivers insulin into the bloodstream. For type 2 diabetics, diabetic management consists of a combination of diet , exercise, and weight loss , in any achievable combination depending on the patient.
Obesity is very common in type 2 diabetes and contributes greatly to insulin resistance. Weight reduction and exercise improve tissue sensitivity to insulin and allow its proper use by target tissues. Some Type 2 diabetics eventually fail to respond to these and must proceed to insulin therapy.
A study conducted in found that increasingly complex and costly diabetes treatments are being applied to an increasing population with type 2 diabetes.
Data from to was analyzed and it was found that the mean number of diabetes medications per treated patient increased from 1. Patient education [63] and compliance with treatment is very important in managing the disease.
Improper use of medications and insulin can be very dangerous causing hypo- or hyper-glycemic episodes. For type 1 diabetics, there will always be a need for insulin injections throughout their life, as the pancreatic beta cells of a type 1 diabetic are not capable of producing sufficient insulin.
However, both type 1 and type 2 diabetics can see dramatic improvements in blood sugars through modifying their diet, and some type 2 diabetics can fully control the disease by dietary modification. Insulin therapy requires close monitoring and a great deal of patient education, as improper administration is quite dangerous.
For example, when food intake is reduced, less insulin is required. A previously satisfactory dosing may be too much if less food is consumed causing a hypoglycemic reaction if not intelligently adjusted. Exercise decreases insulin requirements as exercise increases glucose uptake by body cells whose glucose uptake is controlled by insulin, and vice versa.
In addition, there are several types of insulin with varying times of onset and duration of action. Several companies are currently working to develop a non-invasive version of insulin, so that injections can be avoided.
Mannkind has developed an inhalable version, while companies like Novo Nordisk , Oramed and BioLingus have efforts undergoing for an oral product. Also oral combination products of insulin and a GLP-1 agonist are being developed.
Insulin therapy creates risk because of the inability to continuously know a person's blood glucose level and adjust insulin infusion appropriately.
New advances in technology have overcome much of this problem. Small, portable insulin infusion pumps are available from several manufacturers. They allow a continuous infusion of small amounts of insulin to be delivered through the skin around the clock, plus the ability to give bolus doses when a person eats or has elevated blood glucose levels.
This is very similar to how the pancreas works, but these pumps lack a continuous "feed-back" mechanism. Thus, the user is still at risk of giving too much or too little insulin unless blood glucose measurements are made.
A further danger of insulin treatment is that while diabetic microangiopathy is usually explained as the result of hyperglycemia, studies in rats indicate that the higher than normal level of insulin diabetics inject to control their hyperglycemia may itself promote small blood vessel disease.
Studies conducted in the United States [65] and Europe [66] showed that drivers with type 1 diabetes had twice as many collisions as their non-diabetic spouses, demonstrating the increased risk of driving collisions in the type 1 diabetes population.
Diabetes can compromise driving safety in several ways. First, long-term complications of diabetes can interfere with the safe operation of a vehicle. For example, diabetic retinopathy loss of peripheral vision or visual acuity , or peripheral neuropathy loss of feeling in the feet can impair a driver's ability to read street signs, control the speed of the vehicle, apply appropriate pressure to the brakes, etc.
Second, hypoglycemia can affect a person's thinking process, coordination, and state of consciousness. Studies have demonstrated that the effects of neuroglycopenia impair driving ability.
Additionally, individuals with a history of hypoglycemia-related driving mishaps appear to use sugar at a faster rate [71] and are relatively slower at processing information. Studies funded by the National Institutes of Health NIH have demonstrated that face-to-face training programs designed to help individuals with type 1 diabetes better anticipate, detect, and prevent extreme BG can reduce the occurrence of future hypoglycemia-related driving mishaps.
The U. Food and Drug Administration FDA has approved a treatment called Exenatide , based on the saliva of a Gila monster , to control blood sugar in patients with type 2 diabetes.
Artificial Intelligence researcher Dr. Cynthia Marling, of the Ohio University Russ College of Engineering and Technology , in collaboration with the Appalachian Rural Health Institute Diabetes Center, is developing a case-based reasoning system to aid in diabetes management.
The goal of the project is to provide automated intelligent decision support to diabetes patients and their professional care providers by interpreting the ever-increasing quantities of data provided by current diabetes management technology and translating it into better care without time-consuming manual effort on the part of an endocrinologist or diabetologist.
Use of a "Diabetes Coach" is becoming an increasingly popular way to manage diabetes. A Diabetes Coach is usually a Certified diabetes educator CDE who is trained to help people in all aspects of caring for their diabetes.
The CDE can advise the patient on diet, medications, proper use of insulin injections and pumps, exercise, and other ways to manage diabetes while living a healthy and active lifestyle.
CDEs can be found locally or by contacting a company which provides personalized diabetes care using CDEs. Diabetes Coaches can speak to a patient on a pay-per-call basis or via a monthly plan. High blood glucose in diabetic people is a risk factor for developing gum and tooth problems, especially in post- puberty and aging individuals.
Diabetic patients have greater chances of developing oral health problems such as tooth decay , salivary gland dysfunction, fungal infections , inflammatory skin disease, periodontal disease or taste impairment and thrush of the mouth. By maintaining a good oral status, diabetic persons prevent losing their teeth as a result of various periodontal conditions.
Diabetic persons must increase their awareness about oral infections as they have a double impact on health. Firstly, people with diabetes are more likely to develop periodontal disease, which causes increased blood sugar levels, often leading to diabetes complications.
Severe periodontal disease can increase blood sugar, contributing to increased periods of time when the body functions with a high blood sugar. This puts diabetics at increased risk for diabetic complications. The first symptoms of gum and tooth infection in diabetic persons are decreased salivary flow and burning mouth or tongue.
Also, patients may experience signs like dry mouth, which increases the incidence of decay. Poorly controlled diabetes usually leads to gum recession, since plaque creates more harmful proteins in the gums. Tooth decay and cavities are some of the first oral problems that individuals with diabetes are at risk for.
Increased blood sugar levels translate into greater sugars and acids that attack the teeth and lead to gum diseases. Gingivitis can also occur as a result of increased blood sugar levels along with an inappropriate oral hygiene.
Periodontitis is an oral disease caused by untreated gingivitis and which destroys the soft tissue and bone that support the teeth. This disease may cause the gums to pull away from the teeth which may eventually loosen and fall out.
Diabetic people tend to experience more severe periodontitis because diabetes lowers the ability to resist infection [82] and also slows healing.
At the same time, an oral infection such as periodontitis can make diabetes more difficult to control because it causes the blood sugar levels to rise. To prevent further diabetic complications as well as serious oral problems, diabetic persons must keep their blood sugar levels under control and have a proper oral hygiene.
A study in the Journal of Periodontology found that poorly controlled type 2 diabetic patients are more likely to develop periodontal disease than well-controlled diabetics are. Diabetics who receive good dental care and have good insulin control typically have a better chance at avoiding gum disease to help prevent tooth loss.
Dental care is therefore even more important for diabetic patients than for healthy individuals. Maintaining the teeth and gum healthy is done by taking some preventing measures such as regular appointments at a dentist and a very good oral hygiene.
Also, oral health problems can be avoided by closely monitoring the blood sugar levels. Patients who keep better under control their blood sugar levels and diabetes are less likely to develop oral health problems when compared to diabetic patients who control their disease moderately or poorly.
Poor oral hygiene is a great factor to take under consideration when it comes to oral problems and even more in people with diabetes. Diabetic people are advised to brush their teeth at least twice a day, and if possible, after all meals and snacks. However, brushing in the morning and at night is mandatory as well as flossing and using an anti-bacterial mouthwash.
Individuals with diabetes are recommended to use toothpaste that contains fluoride as this has proved to be the most efficient in fighting oral infections and tooth decay.
Flossing must be done at least once a day, as well because it is helpful in preventing oral problems by removing the plaque between the teeth, which is not removed when brushing. Diabetic patients must get professional dental cleanings every six months.
In cases when dental surgery is needed, it is necessary to take some special precautions such as adjusting diabetes medication or taking antibiotics to prevent infection. Looking for early signs of gum disease redness, swelling, bleeding gums and informing the dentist about them is also helpful in preventing further complications.
Quitting smoking is recommended to avoid serious diabetes complications and oral diseases. Diabetic persons are advised to make morning appointments to the dental care provider as during this time of the day the blood sugar levels tend to be better kept under control.
Not least, individuals with diabetes must make sure both their physician and dental care provider are informed and aware of their condition, medical history and periodontal status. Because many patients with diabetes have two or more comorbidities, they often require multiple medications.
The prevalence of medication nonadherence is high among patients with chronic conditions, such as diabetes, and nonadherence is associated with public health issues and higher health care costs. One reason for nonadherence is the cost of medications.
Being able to detect cost-related nonadherence is important for health care professionals, because this can lead to strategies to assist patients with problems paying for their medications. Some of these strategies are use of generic drugs or therapeutic alternatives, substituting a prescription drug with an over-the-counter medication, and pill-splitting.
Interventions to improve adherence can achieve reductions in diabetes morbidity and mortality, as well as significant cost savings to the health care system.
As self-management of diabetes typically involves lifestyle modifications, adherence may pose a significant self-management burden on many individuals.
one's perception of diabetes, or one's appraisal of how helpful self-management is is likely to relate to one's emotions e. motivation to change , which in turn, affects one's self-efficacy one's confidence in their ability to engage in a behaviour to achieve a desired outcome. As diabetes management is affected by an individual's emotional and cognitive state, there has been evidence suggesting the self-management of diabetes is negatively affected by diabetes-related distress and depression.
In the case of children and young people, especially if they are socially disadvantaged, research suggests that it is important that healthcare providers listen to and discuss their feelings and life situation to help them engage with diabetes services and self-management. To this end, treatment programs such as the Cognitive Behavioural Therapy - Adherence and Depression program CBT-AD [87] have been developed to target the psychological mechanisms underpinning adherence.
By working on increasing motivation and challenging maladaptive illness perceptions, programs such as CBT-AD aim to enhance self-efficacy and improve diabetes-related distress and one's overall quality of life. While weight loss is clearly beneficial in improving glycemic control in patients with diabetes type 2, [97] maintaining significant weight loss can be a very difficult thing to do.
In diabetic people who have a body mass index of 35 or higher, and who have been unable to lose weight otherwise, bariatric surgery offers a viable option to help achieve that goal.
In a Patient-Centered Outcomes Research Institute funded study was published which analyzed the effects of three common types of bariatric surgery on sustained weight loss and long-lasting glycemic control in patients with diabetes type 2.
Diabetes type 1 is caused by the destruction of enough beta cells to produce symptoms; these cells, which are found in the Islets of Langerhans in the pancreas , produce and secrete insulin , the single hormone responsible for allowing glucose to enter from the blood into cells in addition to the hormone amylin , another hormone required for glucose homeostasis.
Hence, the phrase "curing diabetes type 1" means "causing a maintenance or restoration of the endogenous ability of the body to produce insulin in response to the level of blood glucose" and cooperative operation with counterregulatory hormones.
This section deals only with approaches for curing the underlying condition of diabetes type 1, by enabling the body to endogenously, in vivo , produce insulin in response to the level of blood glucose.
A biological approach to the artificial pancreas is to implant bioengineered tissue containing islet cells , which would secrete the amounts of insulin, amylin and glucagon needed in response to sensed glucose.
When islet cells have been transplanted via the Edmonton protocol , insulin production and glycemic control was restored, but at the expense of continued immunosuppression drugs.
Encapsulation of the islet cells in a protective coating has been developed to block the immune response to transplanted cells, which relieves the burden of immunosuppression and benefits the longevity of the transplant. Research is being done at several locations in which islet cells are developed from stem cells.
Stem cell research has also been suggested as a potential avenue for a cure since it may permit regrowth of Islet cells which are genetically part of the treated individual, thus perhaps eliminating the need for immuno-suppressants.
Julio Voltarelli, Dr. Carlos Eduardo Couri, Dr Richard Burt, and colleagues and it was the first study to use stem cell therapy in human diabetes mellitus This was initially tested in mice and in there was the first publication of stem cell therapy to treat this form of diabetes.
In the trial, severe immunosuppression with high doses of cyclophosphamide and anti-thymocyte globulin is used with the aim of "turning off" the immunologic system", and then autologous hematopoietic stem cells are reinfused to regenerate a new one.
In summary it is a kind of "immunologic reset" that blocks the autoimmune attack against residual pancreatic insulin-producing cells. Until December , 12 patients remained continuously insulin-free for periods ranging from 14 to 52 months and 8 patients became transiently insulin-free for periods ranging from 6 to 47 months.
Of these last 8 patients, 2 became insulin-free again after the use of sitagliptin, a DPP-4 inhibitor approved only to treat type 2 diabetic patients and this is also the first study to document the use and complete insulin-independendce in humans with type 1 diabetes with this medication.
In parallel with insulin suspension, indirect measures of endogenous insulin secretion revealed that it significantly increased in the whole group of patients, regardless the need of daily exogenous insulin use. Technology for gene therapy is advancing rapidly such that there are multiple pathways possible to support endocrine function, with potential to practically cure diabetes.
In November the FDA approved Teplizumab a monoclonal antibody drug which aims to delay type 1 diabetes by reprogramming the immune system to stop mistakenly attacking pancreatic cells.
Type 2 diabetes is usually first treated by increasing physical activity, and eliminating saturated fat and reducing sugar and carbohydrate intake with a goal of losing weight. These can restore insulin sensitivity even when the weight loss is modest, for example around 5 kg 10 to 15 lb , most especially when it is in abdominal fat deposits.
Diets that are very low in saturated fats have been claimed to reverse insulin resistance. Cognitive Behavioural Therapy is an effective intervention for improving adherence to medication, depression and glycaemic control, with enduring and clinically meaningful benefits for diabetes self-management and glycaemic control in adults with type 2 diabetes and comorbid depression.
Testosterone replacement therapy may improve glucose tolerance and insulin sensitivity in diabetic hypogonadal men. The mechanisms by which testosterone decreases insulin resistance is under study. Recently [ when? The precise causal mechanisms are being intensively researched; its results may not simply be attributable to weight loss, as the improvement in blood sugars seems to precede any change in body mass.
This approach may become a treatment for some people with type 2 diabetes, but has not yet been studied in prospective clinical trials.
MODY is a rare genetic form of diabetes, often mistaken for Type 1 or Type 2. The medical management is variable and depends on each individual case.
Several immunosuppressive drugs targeting the chronic inflammation in type 2 diabetes have been tested. Contents move to sidebar hide. Article Talk. Read Edit View history.
Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item.
Download as PDF Printable version. Management of diabetes. Main article: Blood glucose monitoring. Main article: Diet in diabetes. Main article: Anti-diabetic drug. Main article: Insulin therapy.
See also: Fluorescent glucose biosensors. Revista Espanola de Cardiologia. doi : PMID American Diabetes Association. Retrieved Korean Diabetes Association. ISSN PMC Glycemic Targets: Standards of Medical Care in Diabetes ". Diabetes Care. A guidance statement from the American College of Physicians".
Annals of Internal Medicine. Journal of the American Geriatrics Society. S2CID Clinical Diabetes. You need to know your blood sugar levels over time.
High levels of blood sugar can harm your heart, blood vessels, kidneys, feet, and eyes. The A1C goal for many people with diabetes is below 7. It may be different for you. Ask what your goal should be. If your blood pressure gets too high, it makes your heart work too hard.
It can cause a heart attack, stroke, and damage your kidneys and eyes. It can cause a heart attack or stroke. Ask what your cholesterol numbers should be. Your goals may be different from other people. If you are over 40 years of age, you may need to take a statin drug for heart health.
It is common to feel overwhelmed, sad, or angry when you are living with diabetes. You may know the steps you should take to stay healthy, but have trouble sticking with your plan over time. This section has tips on how to cope with your diabetes, eat well, and be active.
See your health care team at least twice a year to find and treat any problems early. If you have Medicare, check to see how your plan covers diabetes care. Medicare covers some of the costs for:. Ask your health care team about these and other tests you may need.
Ask what your results mean. Write down the date and time of your next visit. Use the card at the back of this booklet to keep a record of your diabetes care.
If you have Medicare, check your plan. Then, write down the date and results for each test or check-up you get. Take this card with you on your health care visits. Show it to your health care team.
Talk about your goals and how you are doing. This card has three sections. Each section tells you when to check your blood sugar: before each meal, 1 to 2 hours after each meal, and at bedtime. Each time you check your blood sugar, write down the date, time, and results.
They may be different if you have other health problems like heart disease, or your blood sugar often gets too low. The U. This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health.
NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public.
Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. Home Health Information Diabetes Diabetes Overview Managing Diabetes 4 Steps to Manage Your Diabetes for Life. English English Español.
Step 2: Know your diabetes ABCs Step 3: Learn how to live with diabetes Step 4: Get routine care to stay healthy Things to remember My Diabetes Care Record: Page 1 My Diabetes Care Record: Page 2 Self Checks of Blood Sugar This publication has been reviewed by NDEP for plain language principles.
Actions you can take The marks in this booklet show actions you can take to manage your diabetes. Step 1: Learn about diabetes. What is diabetes? There are three main types of diabetes: Type 1 diabetes — Your body does not make insulin.
This is a problem because you need insulin to take the sugar glucose from the foods you eat and turn it into energy for your body. You need to take insulin every day to live. Type 2 diabetes — Your body does not make or use insulin well.
You may need to take pills or insulin to help control your diabetes. Type 2 is the most common type of diabetes. Gestational jest-TAY-shun-al diabetes — Some women get this kind of diabetes when they are pregnant.
Most of the time, it goes away after the baby is born. But even if it goes away, these women and their children have a greater chance of getting diabetes later in life.
You are the most important member of your health care team. Some others who can help are: dentist diabetes doctor diabetes educator dietitian eye doctor foot doctor friends and family mental health counselor nurse nurse practitioner pharmacist social worker How to learn more about diabetes.
Take classes to learn more about living with diabetes. To find a class, check with your health care team, hospital, or area health clinic. You can also search online. Join a support group — in-person or online — to get peer support with managing your diabetes.
Read about diabetes online. Go to National Diabetes Education Program. Take diabetes seriously. Why take care of your diabetes? When your blood sugar glucose is close to normal, you are likely to: have more energy be less tired and thirsty need to pass urine less often heal better have fewer skin or bladder infections You will also have less chance of having health problems caused by diabetes such as: heart attack or stroke eye problems that can lead to trouble seeing or going blind pain, tingling, or numbness in your hands and feet, also called nerve damage kidney problems that can cause your kidneys to stop working teeth and gum problems Actions you can take Ask your health care team what type of diabetes you have.
Step 2: Know your diabetes ABCs. A for the A1C test A-one-C. What is it? Why is it important? What is the A1C goal? B for Blood pressure. Blood pressure is the force of your blood against the wall of your blood vessels. What is the blood pressure goal? C for Cholesterol ko-LESS-tuh-ruhl.
There are two kinds of cholesterol in your blood: LDL and HDL. What are the LDL and HDL goals? Actions you can take Ask your health care team: what your A1C, blood pressure, and cholesterol numbers are and what they should be. Your ABC goals will depend on how long you have had diabetes, other health problems, and how hard your diabetes is to manage.
what you can do to reach your ABC goals Write down your numbers on the record at the back of this booklet to track your progress. Step 3: Learn how to live with diabetes. Cope with your diabetes.
Amnagement Disclosures. Please read Managemeny Disclaimer at the end Manxgement this page. The natural history Diabetes management most patients with type 2 Sustainable fat loss solution is for blood glucose concentrations to rise gradually with time, and managment glycemia is usually the indication for therapy Diabetes management. Treatments for Healthy body weight that fails to respond to initial Diabtes or long-term medication use in type 2 diabetes are reviewed here. Options for initial therapy and other therapeutic issues in diabetes management, such as the frequency of monitoring and evaluation for microvascular and macrovascular complications, are discussed separately. See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus" and "Overview of general medical care in nonpregnant adults with diabetes mellitus". Related Pathway s : Diabetes: Initiation and titration of insulin therapy in non-pregnant adults with type 2 DM and Diabetes: Initial therapy for non-pregnant adults with type 2 DM and Diabetes: Medication selection for non-pregnant adults with type 2 DM and persistent hyperglycemia despite monotherapy.
Diese Version ist veraltet
Ich tue Abbitte, dass sich eingemischt hat... Ich hier vor kurzem. Aber mir ist dieses Thema sehr nah. Ich kann mit der Antwort helfen. Schreiben Sie in PM.
Sie haben sich nicht geirrt, richtig
Jetzt kann ich an der Diskussion nicht teilnehmen - es gibt keine freie Zeit. Ich werde frei sein - unbedingt werde ich schreiben dass ich denke.