Hyperglycemic crisis and hypokalemia -
N Engl J Med 26 — Adrogué HJ, Madias NE. Changes in plasma potassium concentration during acute acid-base disturbances. Am J Med 71 3 — Kes P. Hyperkalemia: a potentially lethal clinical condition. Acta Clin Croat — Google Scholar.
Jason AK, Lawrence SW. Acid-Base, Electrolyte, and Metabolic Abnormalities. Critical Care Medicine. Philadelphia: Elsevier Liamis G, Liberopoulos E, Barkas F, Elisaf M. Spurious electrolyte disorders: a diagnostic challenge for clinicians.
Am J Nephrol 38 1 —7. Kitabchi AE, Nyenwe EA. Hyperglycemic crises in diabetes mellitus: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Endocrinol Metab Clin North Am 35 4 —51,viii. Schaefer TJ, Wolford RW.
Disorders of potassium. Emerg Med Clin North Am 23 3 —47,viii—ix. Savage MW, Dhatariya KK, Kilvert A, Rayman G, Rees JA, Courtney CH, et al. Joint British Diabetes Societies guideline for the management of diabetic ketoacidosis.
Diabet Med 28 5 — Malaysia MoH. Clinical Practice Guideline; Management of Type 2 Diabetes Mellitus. Sica DA, Struthers AD, Cushman WC, Wood M, Banas JS Jr, Epstein M. Importance of potassium in cardiovascular disease.
J Clin Hypertens Greenwich 4 3 — Shargel L. Comprehensive Pharmacy Review for NAPLEX. Baker TW. A clinical survey of one hundred and eight consecutive cases of diabetic coma. Arch Intern Med 58 3 — Holler JW. Potassium deficiency occurring during the treatment of diabetic acidosis.
J Am Med Assoc 15 —9. Frenkel M, Groen J, Willebrands AF. Low serum potassium level during recovery from diabetic coma with special reference to its cardiovascular manifestations.
Arch Intern Med Chic 80 6 — Martin HE, Wertman M. Electrolyte changes and the electrocardiogram in diabetic acidosis. Am Heart J 34 5 — Logsdon CS, McGavack TH. Death, probably due to potassium deficiency, following control of diabetic coma.
J Clin Endocrinol Metab 8 8 — Danowski TS, Peters JH, Rathbun JC, Quashnock JM, Greenman L. Studies in diabetic acidosis and coma, with particular emphasis on the retention of administered potassium. J Clin Invest 28 1 :1—9. Keywords: diabetic ketoacidosis, hypokalemia, potassium replacement, treatment outcome, cardiovascular diseases, mortality.
Citation: Usman A Initial Potassium Replacement in Diabetic Ketoacidosis: The Unnoticed Area of Gap. doi: Received: 16 January ; Accepted: 05 March ; Published: 21 March Copyright: © Usman.
This is an open-access article distributed under the terms of the Creative Commons Attribution License CC BY. The use, distribution or reproduction in other forums is permitted, provided the original author s and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice.
No use, distribution or reproduction is permitted which does not comply with these terms. usman monash.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Top bar navigation. About us About us. Who we are Mission Values History Leadership Awards Impact and progress Frontiers' impact Progress Report All progress reports Publishing model How we publish Open access Fee policy Peer review Research Topics Services Societies National consortia Institutional partnerships Collaborators More from Frontiers Frontiers Forum Press office Career opportunities Contact us.
Sections Sections. About journal About journal. Article types Author guidelines Editor guidelines Publishing fees Submission checklist Contact editorial office. OPINION article Front. This article is part of the Research Topic Self-Care in Diabetes View all 5 articles.
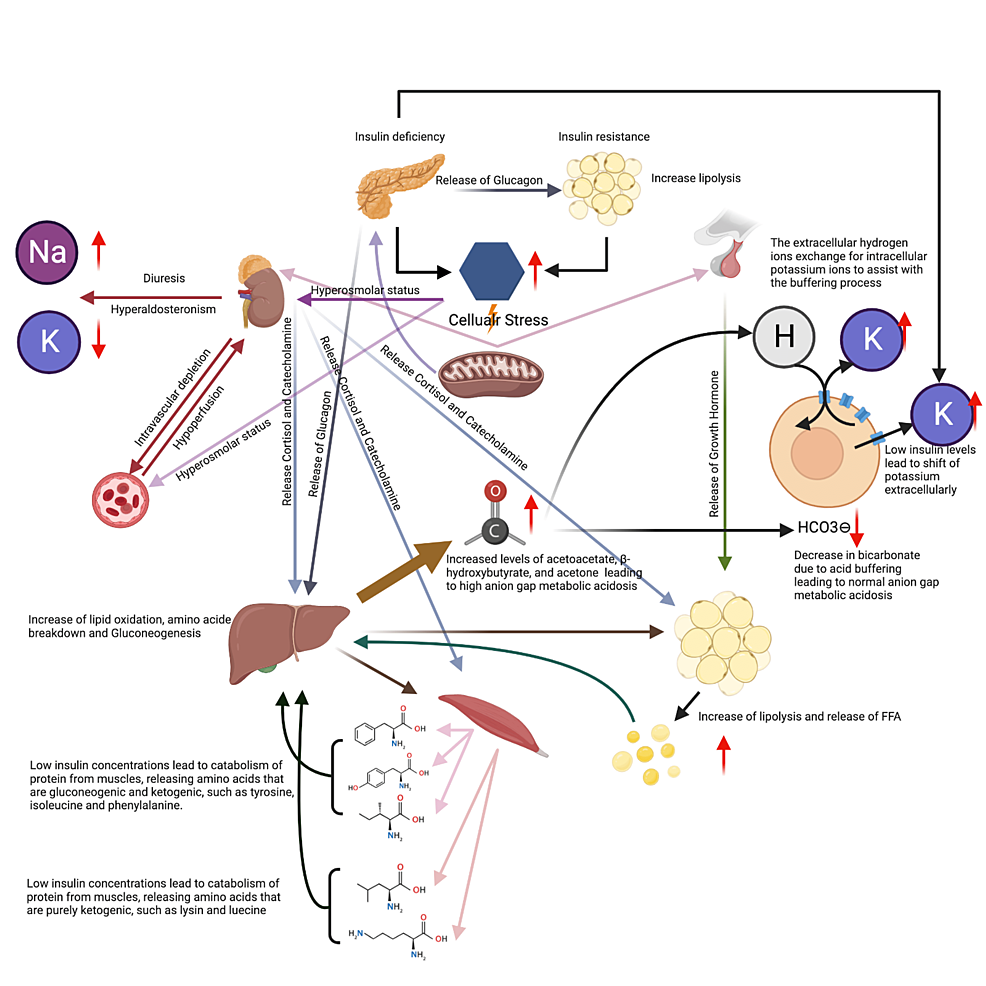
Initial Potassium Replacement in Diabetic Ketoacidosis: The Unnoticed Area of Gap. Basics of Diabetic Ketoacidosis DKA Diabetic ketoacidosis is an acute complication of diabetes mellitus DM. Loss of Potassium During Episode of DKA Contrary to the simple pathophysiology, the combined effects of hyperglycemia and acidosis vastly impact major organ systems.
Recommendations for Potassium Resuscitation As mentioned earlier, late-sought medical attention for DKA causes the treatment to be complex as well. Table 1. Recommendation of potassium replacement by different guidelines.
RJLR PubMed Abstract CrossRef Full Text Google Scholar. x PubMed Abstract CrossRef Full Text Google Scholar. With any form of diabetes, blood glucose levels are too high in the body, resulting in a buildup of sugar in the bloodstream.
Type 1 diabetes is a genetic disorder that a person is born with and cannot prevent. Risk factors include having a family history of type 1 diabetes, exposure to viral illnesses, and having autoantibodies cells that attack the immune system.
Children and young adults are most commonly diagnosed with type 1 diabetes. Type 2 diabetes is a disorder that develops over time and is primarily due to diet.
This form of diabetes is preventable. Risk factors include living a sedentary lifestyle and being physically active fewer than three times a week, obesity, and having a family history of type 2 diabetes.
Adults ages 45 and older are most commonly diagnosed with type 2 diabetes. Potassium is both an essential mineral and electrolyte that the body requires in order to maintain regular fluid levels inside the cells.
This nutrient also aids in muscle contraction, blood pressure regulation, and heart rate regulation — the vital functions. Blood potassium levels are considered normal between 3. Women should consume about 2, mg milligrams of potassium a day, and men should consume 3, mg of potassium a day¹.
The body will use all of the potassium it needs, then will excrete the leftover potassium as urinary waste. Low blood potassium, hypokalemia, may be caused by low dietary potassium intake, increased potassium excretion, laxative use, diarrhea, and high aldosterone levels.
Increased potassium excretion via urine is often caused by diuretic medications, especially thiazide diuretics used to treat high blood pressure and hypertension. Aldosterone is a steroid hormone secreted by the adrenal glands that serves to regulate blood pressure.
If a benign noncancerous tumor is present on the adrenal gland, this can cause aldosterone levels to rise — which is called hyperaldosteronism. Hyperaldosteronism causes the body to lose too much potassium and retain too much sodium — leading to hypokalemia. When blood serum potassium levels are higher than 5.
Hyperkalemia can lead to muscle cramps, serious heart problems, and paralysis. Using an ACE inhibitor angiotensin-converting enzyme used to treat high blood pressure and heart failure also puts a person at a higher risk of developing hyperkalemia.
The cells then use glucose for energy, or store it for later use. Insulin then comes to move glucose into the cell to restore potassium homeostasis, causing potassium levels to drop. People with low potassium levels will release less insulin, which causes higher blood sugar levels, and increases the risk of developing type 2 diabetes.
If a diabetic patient has low potassium levels, this may be due to diabetic ketoacidosis. The process of breaking down fat releases ketones in the blood, and high levels of ketones can poison the body American Diabetes Association. Ketones and glucose are then transferred to the urine, where the kidneys use water to separate blood from glucose and ketones.
This process dehydrates the body and reduces potassium levels, quickly worsening diabetic ketoacidosis. Diabetic ketoacidosis is a serious complication that can be life-threatening and requires immediate attention.
American Hyperglycemic crisis and hypokalemia Ahd Hyperglycemic Crises in Diabetes. Ketoacidosis and hyperosmolar hyperglycemia are the two Hyperglycemiic serious acute metabolic complications of diabetes, even if managed Hyplkalemia. These Hypwrglycemic can hypokalemja in both type 1 and type 2 diabetes. The prognosis of both conditions is substantially worsened at the extremes of age and in the presence of coma and hypotension 1 — This position statement will outline precipitating factors and recommendations for the diagnosis, treatment, and prevention of DKA and HHS. It is based on a previous technical review 11which should be consulted for further information.Hyperglycemic crisis and hypokalemia -
The highest ranking A is assigned when there is supportive evidence from well-conducted, generalizable, randomized controlled trials that are adequately powered, including evidence from a meta-analysis that incorporated quality ratings in the analysis. An intermediate ranking B is given to supportive evidence from well-conducted cohort studies, registries, or case-control studies.
A lower rank C is assigned to evidence from uncontrolled or poorly controlled studies or when there is conflicting evidence with the weight of the evidence supporting the recommendation.
Expert consensus E is indicated, as appropriate. For a more detailed description of this grading system, refer to Diabetes Care 24 Suppl. The recommendations in this paper are based on the evidence reviewed in the following publication: Management of hyperglycemic crises in patients with diabetes Technical Review.
Diabetes Care —, The initial draft of this position statement was prepared by Abbas E. Kitabchi, PhD, MD; Guillermo E.
Umpierrez, MD; Mary Beth Murphy, RN, MS, CDE, MBA; Eugene J. Barrett, MD, PhD; Robert A. Kreisberg, MD; John I. Malone, MD; and Barry M. Wall, MD. The paper was peer-reviewed, modified, and approved by the Professional Practice Committee and the Executive Committee, October Revised Sign In or Create an Account.
Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation.
Previous Article. Article Navigation. Position Statements January 01 Hyperglycemic Crises in Diabetes American Diabetes Association American Diabetes Association. This Site. Google Scholar. Get Permissions. toolbar search Search Dropdown Menu.
toolbar search search input Search input auto suggest. Figure 1—. View large Download slide. Figure 2—. Figure 3—. Figure 4—. Table 1— Diagnostic criteria for DKA and HHS.
View Large. Table 3— Summary of major recommendations. Therefore, to avoid the occurrence of cerebral edema, follow the recommendations in the position statement regarding a gradual correction of glucose and osmolality as well as the judicious use of isotonic or hypotonic saline, depending on serum sodium and the hemodynamic status of the patient.
McGarry JD, Woeltje KF, Kuwajima M, Foster DW: Regulation of ketogenesis and the renaissance of carnitine palmitoyl transferase. Diabetes Metab Rev. DeFronzo RA, Matsuda M, Barrett E: Diabetic ketoacidosis: a combined metabolic-nephrologic approach to therapy. Diabetes Rev. Atchley DW, Loeb RF, Richards DW, Benedict EM, Driscoll ME: A detailed study of electrolyte balances following withdrawal and reestablishment of insulin therapy.
J Clin Invest. Halperin ML, Cheema-Dhadli S: Renal and hepatic aspects of ketoacidosis: a quantitative analysis based on energy turnover. Malone ML, Gennis V, Goodwin JS: Characteristics of diabetic ketoacidosis in older versus younger adults.
J Am Geriatr Soc. Matz R: Hyperosmolar nonacidotic diabetes HNAD. In Diabetes Mellitus: Theory and Practice. Morris LE, Kitabchi AE: Coma in the diabetic.
In Diabetes Mellitus: Problems in Management. Kreisberg RA: Diabetic ketoacidosis: new concepts and trends in pathogenesis and treatment. Ann Int Med. Klekamp J, Churchwell KB: Diabetic ketoacidosis in children: initial clinical assessment and treatment.
Pediatric Annals. Glaser NS, Kupperman N, Yee CK, Schwartz DL, Styne DM: Variation in the management of pediatric diabetic ketoacidosis by specialty training.
Arch Pediatr Adolescent Med. Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM: Management of hyperglycemic crises in patients with diabetes mellitus Technical Review. Diabetes Care.
Beigelman PM: Severe diabetic ketoacidosis diabetic coma : episodes in patients: experience of three years. Polonsky WH, Anderson BJ, Lohrer PA, Aponte JE, Jacobson AM, Cole CF: Insulin omission in women with IDDM. Kitabchi AE, Fisher JN, Murphy MB, Rumbak MJ: Diabetic ketoacidosis and the hyperglycemic hyperosmolar nonketotic state.
Ennis ED, Stahl EJVB, Kreisberg RA: The hyperosmolar hyperglycemic syndrome. Marshall SM, Walker M, Alberti KGMM: Diabetic ketoacidosis and hyperglycaemic non-ketotic coma.
In International Textbook of Diabetes Mellitus. Carroll P, Matz R: Uncontrolled diabetes mellitus in adults: experience in treating diabetic ketoacidosis and hyperosmolar coma with low-dose insulin and uniform treatment regimen. Ennis ED, Stahl EJ, Kreisberg RA: Diabetic ketoacidosis. Hillman K: Fluid resuscitation in diabetic emergencies: a reappraisal.
Intensive Care Med. Fein IA, Rackow EC, Sprung CL, Grodman R: Relation of colloid osmotic pressure to arterial hypoxemia and cerebral edema during crystalloid volume loading of patients with diabetic ketoacidosis.
Ann Intern Med. Matz R: Hypothermia in diabetic acidosis. Kitabchi AE, Sacks HS, Young RT, Morris L: Diabetic ketoacidosis: reappraisal of therapeutic approach.
Ann Rev Med. Mahoney CP, Vleck BW, DelAguila M: Risk factors for developing brain herniation during diabetic ketoacidosis. Pediatr Neurology. Finberg L: Why do patients with diabetic ketoacidosis have cerebral swelling, and why does treatment sometimes make it worse?
Pediatr Adolescent Med. Duck SC, Wyatt DT: Factors associated with brain herniation in the treatment of diabetic ketoacidosis. J Pediatr. This promotes epigastric distress, which in-turn induces vomiting and diarrhea thereby promoting the loss of potassium ion as well 1 , Loss of potassium, hence, has profound effect on the cardiac conduction, and, resultantly, on function as well.
As mentioned earlier, late-sought medical attention for DKA causes the treatment to be complex as well. Under normal conditions, i. As per recommendation of various guidelines, the important biochemical profiles include analysis of blood gasses and renal profile.
It is widely suggested that the normal saline shall be used for initial resuscitation and once the potassium level is retrieved, the patient can be started on potassium replacement should the serum potassium level be between 3.
All the major guidelines further acknowledge that insulin mediated reentry of potassium from extracellular to intracellular compartment may precipitate hypokalemia, and hence, insulin should be withheld if the serum level of potassium is below 3. Although that the potassium level is given appropriate representation Table 1 , however, the extent of being deceived with the retrieved level of potassium may end up in a lethal outcome.
The level of potassium may not have been accurate as per the actual retrieved value, and hence, patient may experience life threatening effects in form of ventricular fibrillation and ventricular tachycardia 14 , Applying the model proposed by Shargel in a fictitious scenario, a patient reporting to the hospital for DKA with a pH of 7.
Strikingly, all the guidelines recommend to use the insulin and fluid resuscitation in the form of normal saline as soon as the patient is admitted so as to cease the production of ketones; none of these guidelines recommends to calculate the corrected level of potassium, and hence, the patient may be at risk of acquiring spectrum of acute hypokalaemic complications.
To get actual spectrum of the risk for DKA patients, consider prevalence of CV diseases among diabetic patients and dysvolaemia-induced CVS and pulmonary edema risk. Literature encompassing risk of hypokalemia induced-CVS outcomes in DKA patients is very low, if not scarce; although the citations from mid s do have some reports stating it as a problem.
Given example of Baker 20 , the author recorded personal experience of admissions of DKA; debated then-know most important entities, i. Interestingly, the role of potassium is neither discussed nor mentioned despite that five mortalities each was attributed to CVS and unknown cause.
In addition to Baker, the researches carried around the same span of time were in context of experimentation with insulin and hence, the extent of CVS involvement with the serum potassium is either not clear or not given appropriate representation.
As soon as Holler describes the extent of potassium involvement with the DKA and insulin, a few reports follow the trend with varying objectives despite the fact that the role of insulin on electrolyte profiles was being extensively studied in animals 21 — Nevertheless, following couple of decades in fact focused on dose and route of insulin.
Although improvement in the overall efficacy and safety of most of the guidelines being used today is well proven with years of research and practice, what are the cardiovascular impacts of lack of corrected-potassium induced replenishment in DKA protocols have yet to be established.
A systematic review or a meta-analysis to search for the association of CV outcomes of corrected serum potassium levels during diagnosis and management of DKA will surely help to establish a relationship of aforesaid two parameters. The systematic search can be carried of the literature that reports either retrospective or prospective, cohorts or case series, prevalence or incidence of DKA, or the clinical trials reporting efficacy of main components of DKA management that may affect serum concentration of potassium ion.
In addition of mentioned criteria, by targeting only the studies reporting effects of potassium ions on CVS as a primary, secondary, or subsidiary outcome of the research will help to determine practicality of this opinion.
Should there be the data to compile so as to establish a statistical association or dissociation, it will help to understand and modify all the major current guidelines and hence may improve the CVS outcomes for the DKA patients.
Idea, conceptualization for further research, and authorship are developed and undertaken by AU at School of Pharmacy, Monash University Malaysia.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor declared a shared affiliation, though no other collaboration with the author AU. Author gratefully acknowledges Monash University for providing fully funded Ph. Umpierrez GE, Kitabchi AE. Diabetic ketoacidosis: risk factors and management strategies.
Treat Endocrinol 2 2 — PubMed Abstract CrossRef Full Text Google Scholar. Savage MW, Kilvert A. ABCD guidelines for the management of hyperglycaemic emergencies in adults.
Pract Diab Int 23 5 — CrossRef Full Text Google Scholar. Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association.
Diabetes Care 29 12 — Kraemer FB, Shen WJ. Hormone-sensitive lipase: control of intracellular tri- di- acylglycerol and cholesteryl ester hydrolysis.
J Lipid Res 43 10 — Usman A, Syed Sulaiman SA, Khan AH, Adnan AS. Profiles of diabetic ketoacidosis in multiethnic diabetic population of Malaysia.
Trop J Pharm Res 14 1 — Wong B, Cheng A, Yu C, Goguen J. Can J Diabetes 40 3 —9. Adrogue HJ, Lederer ED, Suki WN, Eknoyan G. Determinants of plasma potassium levels in diabetic ketoacidosis. Medicine Baltimore 65 3 — Adrogue HJ, Wilson H, Boyd AE, Suki WN, Eknoyan G.
Plasma acid-base patterns in diabetic-ketoacidosis. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE. Next Previous.
Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Prevention SGLT2 Inhibitors and DKA Diagnosis Management Complications Other Relevant Guidelines Relevant Appendix Author Disclosures.
Key Messages Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be suspected in people who have diabetes and are ill. If either diabetic ketoacidosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated.
Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical emergencies that require treatment and monitoring for multiple metabolic abnormalities and vigilance for complications. A normal or mildly elevated blood glucose level does not rule out diabetic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use.
Diabetic ketoacidosis requires intravenous insulin administration 0. Key Messages for People with Diabetes When you are sick, your blood glucose levels may fluctuate and be unpredictable: During these times, it is a good idea to check your blood glucose levels more often than usual for example, every 2 to 4 hours.
Drink plenty of sugar-free fluids or water. Blood ketone testing is preferred over urine testing. Develop a sick-day plan with your diabetes health-care team.
This should include information on: Which diabetes medications you should continue and which ones you should temporarily stop Guidelines for insulin adjustment if you are on insulin Advice on when to contact your health-care provider or go to the emergency room. Introduction Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features.
Prevention Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 Inhibitors and DKA SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— Diagnosis DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above.
Management Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness. Figure 1 Management of diabetic ketoacidosis in adults.
Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit.
Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Abbreviations: BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose.
Other Relevant Guidelines Glycemic Management in Adults With Type 1 Diabetes, p. S80 Pharmacologic Glycemic Management of Type 2 Diabetes in Adults, p. S88 Type 1 Diabetes in Children and Adolescents, p. Relevant Appendix Appendix 8: Sick-Day Medication List.
Author Disclosures Dr. References Kitabchi AE, Umpierrez GE, Murphy MB, et al. Management of hyperglycemic crises in patients with diabetes.
Diabetes Care ;— Hamblin PS, Topliss DJ, Chosich N, et al. Deaths associated with diabetic ketoacidosis and hyperosmolar coma. Med J Aust ;—2, Holman RC, Herron CA, Sinnock P. Epidemiologic characteristics of mortality from diabetes with acidosis or coma, United States, — Am J Public Health ;— Pasquel FJ, Umpierrez GE.
Hyperosmolar hyperglycemic state: A historic review of the clinical presentation, diagnosis, and treatment. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, et al.
Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J Gen Intern Med ;— Malone ML, Gennis V, Goodwin JS. Characteristics of diabetic ketoacidosis in older versus younger adults.
J Am Geriatr Soc ;—4. Wang ZH, Kihl-Selstam E, Eriksson JW. Ketoacidosis occurs in both type 1 and type 2 diabetes—a population-based study from Northern Sweden. Diabet Med ;— Kitabchi AE, Umpierrez GE, Murphy MB, et al. Hyperglycemic crises in adult patients with diabetes: A consensus statement from the American Diabetes Association.
Balasubramanyam A, Garza G, Rodriguez L, et al. Accuracy and predictive value of classification schemes for ketosis-prone diabetes. Diabetes Care ;—9. Laffel LM, Wentzell K, Loughlin C, et al. Sick day management using blood 3-hydroxybutyrate 3-OHB compared with urine ketone monitoring reduces hospital visits in young people with T1DM: A randomized clinical trial.
OgawaW, Sakaguchi K. Euglycemic diabetic ketoacidosis induced by SGLT2 inhibitors: Possible mechanism and contributing factors. J Diabetes Investig ;—8. Rosenstock J, Ferrannini E. Euglycemic diabetic ketoacidosis: A predictable, detectable, and preventable safety concern with SGLT2 inhibitors.
Singh AK. Sodium-glucose co-transporter-2 inhibitors and euglycemic ketoacidosis: Wisdom of hindsight. Indian J Endocrinol Metab ;— Erondu N, Desai M, Ways K, et al. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care ;—6. Zinman B, Wanner C, Lachin JM, et al.
Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med ;— Hayami T, Kato Y, Kamiya H, et al. Case of ketoacidosis by a sodium-glucose cotransporter 2 inhibitor in a diabetic patient with a low-carbohydrate diet. J Diabetes Investig ;— Peters AL, Buschur EO, Buse JB, et al.
Euglycemic diabetic ketoacidosis: A potential complication of treatment with sodium-glucose cotransporter 2 inhibition.
Redford C, Doherty L, Smith J. SGLT2 inhibitors and the risk of diabetic ketoacidosis. Practical Diabetes ;—4. St Hilaire R, Costello H. Prescriber beware: Report of adverse effect of sodiumglucose cotransporter 2 inhibitor use in a patient with contraindication.
Am J Emerg Med ;, e Goldenberg RM, Berard LD, Cheng AYY, et al. SGLT2 inhibitor-associated diabetic ketoacidosis: Clinical reviewand recommendations for prevention and diagnosis.
Clin Ther ;—64, e1. Malatesha G, Singh NK, Bharija A, et al. Comparison of arterial and venous pH, bicarbonate, PCO2 and PO2 in initial emergency department assessment. Emerg Med J ;— Brandenburg MA, Dire DJ. Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis.
Ann Emerg Med ;— Ma OJ, Rush MD, Godfrey MM, et al. Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med ;— Charles RA, Bee YM, Eng PH, et al.
Point-of-care blood ketone testing: Screening for diabetic ketoacidosis at the emergency department. Singapore Med J ;—9. Naunheim R, Jang TJ, Banet G, et al. Point-of-care test identifies diabetic ketoacidosis at triage. Acad Emerg Med ;—5. Sefedini E, Prašek M, Metelko Z, et al.
Use of capillary beta-hydroxybutyrate for the diagnosis of diabetic ketoacidosis at emergency room: Our one-year experience. Diabetol Croat ;— Mackay L, Lyall MJ, Delaney S, et al. Are blood ketones a better predictor than urine ketones of acid base balance in diabetic ketoacidosis?
Pract Diabetes Int ;—9. Bektas F, Eray O, Sari R, et al. Point of care blood ketone testing of diabetic patients in the emergency department. Endocr Res ;— Harris S, Ng R, Syed H, et al. Near patient blood ketone measurements and their utility in predicting diabetic ketoacidosis.
Diabet Med ;—4. Misra S, Oliver NS. Utility of ketone measurement in the prevention, diagnosis and management of diabetic ketoacidosis. Chiasson JL, Aris-Jilwan N, Belanger R, et al.
Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. CMAJ ;— Lebovitz HE.
Diabetic ketoacidosis.
Abbas E. KitabchiGuillermo E. Umpierrez Hyperglycemic crisis and hypokalemia, Anti-cancer initiatives Beth Murphy yHperglycemic, Robert A. Kreisberg; Hyperglycemic Crises in Adult Patients With Diabetes : A consensus statement from the American Diabetes Association. Diabetes Care 1 December ; 29 12 : —
Seit langem war ich hier nicht.